Are Travel Healthcare Social Media Groups Too Toxic?

Social media is a pillar of many people’s daily lives in spite of numerous controversies over the years. Currently, 68 percent of adult Americans use some type of social media, and a majority of them use it on a daily basis, according to data from the Pew Research Center. Daily social media use mirrors the original goal of the platform for many—to help them stay connected with their friends, family and loved ones, and to share their experiences with them. This is emphasized even further in the travel healthcare community, as travelers have an added incentive to use social media platforms. It not only lets them stay in touch with their friends and family on the road, but it provides a platform to network and share knowledge with a vast number of their travel colleagues on a daily basis. “I use Facebook the most for sure,” said Kayla Jones, a travel certified surgical technologist. “I would say mostly because of my job. I’m away from my boyfriend and my family and all of that so I use it to keep up with them. I’m part of a couple of different traveler groups obviously, and I’m also part of scrub tech groups so I use it for…keeping up my knowledge for my next assignment.” Despite these benefits, that same Pew Research Center study found a majority of adults say they would have no problem giving up social media entirely, and many have begun reducing their use of Facebook. It’s easy to assume the decline in usage is related to the barrage of privacy scandals that have hit Facebook, Twitter and other platforms in recent years, but several travel healthcare professionals have pointed to a different issue entirely. Toxicity on social media is not a new problem—studies have shown that social media has a negative effect on mental health—but some say it’s an even greater problem in the travel healthcare community, where a combination of career stress, misinformation, and a mixing of generations can cause a perfect storm of angry posts and nasty comments. “Sometimes it’s too toxic,” Jones said. “I have to close my computer.” Travel nurse Alex McCoy, who manages both a Facebook page and a social Facebook group for her blog website, Fit Travel Life, has reduced her daily social media use to avoid getting caught up in general travel group discussions, she said. “People have started to realize how unhealthy parts of social media can be, and this is across the board,” McCoy said. “It’s a time suck and can cause a lot of negativity, so I see more people talking about filtering.” The Platform: Facebook reigns supreme Social media use is ubiquitous, but not all of the platforms are equal. Facebook still reigns as the most popular social media platform by a wide margin, despite seeing a decline users last year for the first time since 2008. For travelers, one major appeal for using Facebook over competing platforms like Instagram, LinkedIn, Twitter or Snapchat is the ability to form groups. Groups can be created by any Facebook user and provide a public or private space for people to connect through shared interests. Use of groups grew rapidly in 2018, after Facebook changed its algorithm to encourage users to engage more with groups and friends instead of businesses or brands. Healthcare professionals have their choice of numerous different traveler-oriented groups, which range in size from a few dozen users to tens of thousands of members. The focus points of travel healthcare groups also vary greatly, from catch-all travel nursing discussion forums to hyper-specific premium job boards. LinkedIn has also offered a Groups function since 2004, but there are noticeably less groups on the platform targeted at or created by travel healthcare professionals. Thomas Piper, a travel nurse and admin for his own group Scrub Squad 1978, said he’s experimenting more with LinkedIn and Instagram but still prefers Facebook because there’s a lower barrier of entry to communicating with others. “You can connect more,” Piper said. “People don’t have to subscribe to your Instagram, and you can get more information and more messages across that way.” Alex McCoy prefers Instagram to Facebook because of its focus on photo and video content, but agreed that Facebook offers the best tools to connect directly with others. “Instagram can be good for connecting but there is just not really the capability of creating communities,” McCoy said. “It can be hard to get ahold of people. I have tried to connect with people on Instagram and they literally just don’t see my messages because we aren’t following each other so that makes it harder to connect unless you are commenting on posts.” The Problem: Stress, separation and a lack of information Researchers, bloggers and many others have tried to identify the reasons behind social media toxicity with varying conclusions. Some have pointed to the growing political discord surrounding the upcoming 2020 presidential election, while others have aimed the blame at the “commoditization” of likes, comments and shares. Travelers and Facebook group moderators brought up several specific issues that they felt either contribute to the problem of social media toxicity—or make it worse. Picking a target Personal attacks aimed at a person, staffing agency, or healthcare facility came up as the most common type of toxic or negative posts in travel healthcare social media groups. “There are different levels,” said Andrew Craig, a former travel nurse who runs the Traveler Talk Facebook group and website. “The most subtle version of that is simply a sarcastic or condescending comment. We like to think it’s just a comment but in reality, it can affect the other person on the other side of the screen in a physical and emotional way.” Most agreed heated debates are not a problem. Discussions, even when people don’t agree, can be helpful for the community at-large, Kayla Jones said. The discussion crosses into toxic territory when it devolves into targeted, angry comments. “That’s kind of where things on Facebook and
New Report Weighs Costs, Benefits Of Vermont Joining Nursing Compact

Vermont’s Office of Professional Regulation released a new report that found the state could see many benefits from joining the Nursing Licensure Compact, but also noted the change would have a large financial impact. Sen. Virginia Lyons introduced a nursing compact licensure bill on February 22 which would allow for Vermont to join the NLC. If approved, Vermont would become the 32nd state to join the compact. Registered nurses and licensed practical nurses from Vermont nurses could obtain a compact license, and current out-of-state compact license holders could work in Vermont without paying for a single-state license. In terms of regional impact, Vermont nurses would have easier access to New Hampshire and Maine, which are current NLC member states, and potentially Massachusetts, which also has NLC legislation in the works. The report found the benefits of joining the NLC “large and singular.” “The removal of the licensure barrier to practice in Compact States carries particular benefits for traveling nurses and military spouses, as well as in cases of disaster, labor action, or other surges in demand for nurse inflow,” the report finds. “Compact licensing also facilitates e-health and telehealth access, thereby improving the continuity of care.” The report also noted improving license mobility could potentially relieve pressure on healthcare facilities caused by nursing shortages, specifically during emergency situations. “If Vermont joins the eNLC, nurses from other Compact States will be able to provide services in Vermont without encountering the deterrent of obtaining an additional license,” the report finds. “Without these barriers to practice, nurses may be more likely to fill nursing vacancies in Vermont; however we find no studies or other data conclusively demonstrating that participation in the eNLC will alleviate state nursing shortages.” Potential costs of joining the NLC include a hit to the state nursing board’s annual revenue. The report estimated about 4,705 RNs and LPNs would no longer need a single-state license, which would cause a loss of nearly $1 million from the board’s $4 million annual revenue. “Nurses seeking Vermont-only licenses are likely to see licensing fees increase as these licensees bear a greater proportion of the State licensing administration and enforcement costs,” the report finds. “Due to the anticipated revenue loss the Office can forecast that prior to Compact adoption or shortly thereafter the Office will need to see a fee increase in this profession even after the proposed fee increase in the 2019 Legislative Session.” The current annual renewal fee for Vermont state RN and LPN licenses are $140, but if the proposed fee increase and NLC legislation are approved, the report estimates license costs will jump to $280 for RNs and $245 for LPNs. The report also pointed to costs in other areas, including increased administrative needs, staffing needs, the adaptation of licensing software, and the annual $6,000 membership fee owed to the National Council of State Boards of Nursing. Members of the state nursing board voted in support of the state joining the NLC in 2017, and the report noted many of the state’s nurses and major healthcare organizations support the legislation as well. The full report can be viewed here.
New York Nurses Set April Strike Date At 3 Hospital Systems

Registered nurses at three New York healthcare systems issued a 10-day strike notice on Monday, amid claims of unsafe working conditions caused by inadequate staffing, according to a recent union press release. New York State Nurses Association members delivered the strike notice to New York-Presbyterian Hospital, Montefiore, and Mount Sinai hospitals and set the strike date for April 2. The strike could affect more than 10,000 nurses at the three hospitals, according to the union, which have been in contract negotiations for several months with the New York City Hospital Alliance. More than 8,000 members of the nurses union voted earlier this month to authorize a strike if necessary. Union contracts at the facilities ended on December 31, but both parties have met about 30 times at barganing sessions with limited progress, according to an ABC 7 NY report. “Now is the time that all New Yorkers must have what they need and deserve,” Robin Krinsky, RN, NYSNA Board Member and negotiating committee member at Mount Sinai, said in a NYSNA Facebook post. “Safe patient care by educated professional nurses who know how to provide excellent care each and every time a patient requires it.” The union claims nurses are working with anywhere from 9 to 10 patients at at once, and has protested in support of legislation that would establish mandated nurse-to-patient ratios. A “Safe Staffing For Quality Care Act” bill that would establish mandated ratios statewide was reintroduced during this year’s legislative session, and is currently in committee for review. Advocates have pushed for mandated ratios since 2009, when a version of the bill was first introduced.
Death By 1,000 Clicks: Where Electronic Health Records Went Wrong (KHN)
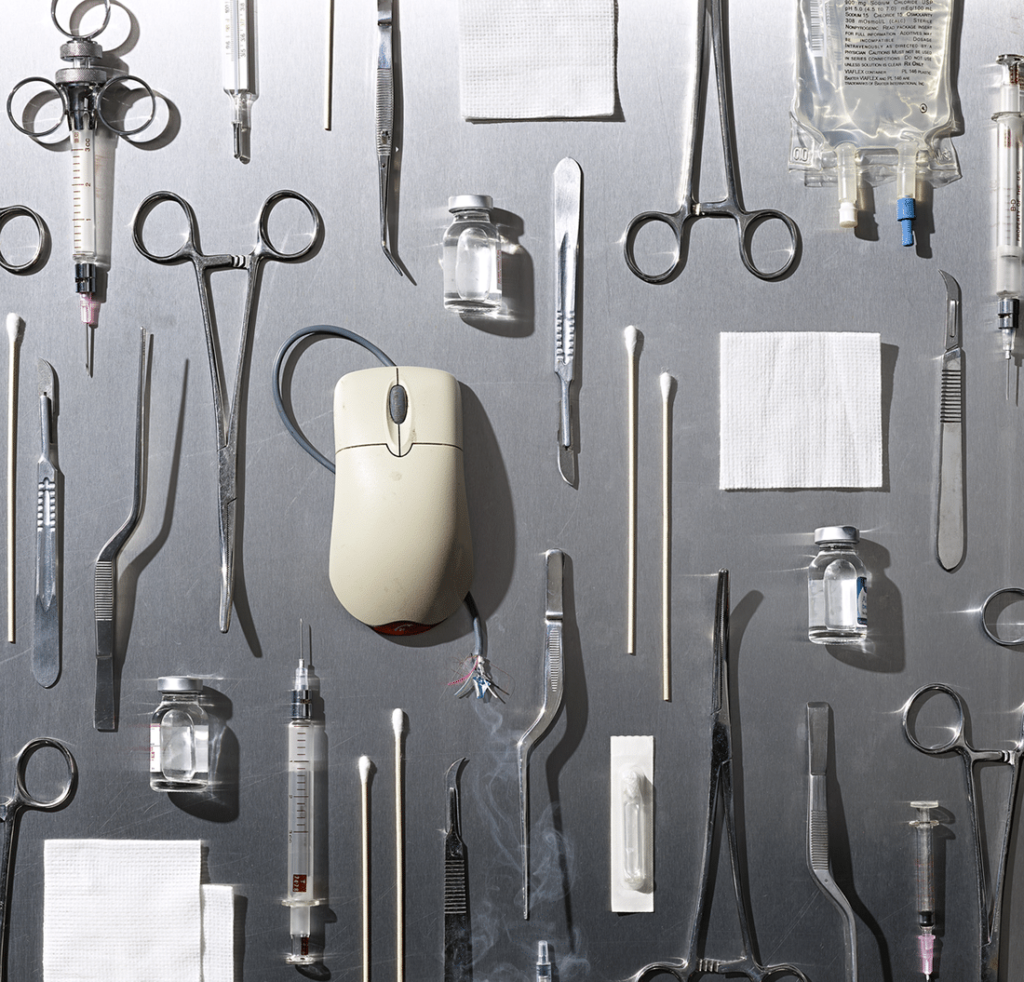
By Fred Schulte, Kaiser Health News and Erika Fry, Fortune The pain radiated from the top of Annette Monachelli’s head, and it got worse when she changed positions. It didn’t feel like her usual migraine. The 47-year-old Vermont attorney turned innkeeper visited her local doctor at the Stowe Family Practice twice about the problem in late November 2012, but got little relief. Two months later, Monachelli was dead of a brain aneurysm, a condition that, despite the symptoms and the appointments, had never been tested for or diagnosed until she turned up in the emergency room days before her death. Monachelli’s husband sued Stowe, the federally qualified health center the physician worked for. Owen Foster, a newly hired assistant U.S. attorney with the District of Vermont, was assigned to defend the government. Though it looked to be a standard medical malpractice case, Foster was on the cusp of discovering something much bigger — what his boss, U.S. Attorney Christina Nolan, calls the “frontier of health care fraud” — and prosecuting a first-of-its-kind case that landed the largest-ever financial recovery in Vermont’s history. Foster began with Monachelli’s medical records, which offered a puzzle. Her doctor had considered the possibility of an aneurysm and, to rule it out, had ordered a head scan through the clinic’s software system, the government alleged in court filings. The test, in theory, would have caught the bleeding in Monachelli’s brain. But the order never made it to the lab; it had never been transmitted. The software in question was an electronic health records system, or EHR, made by eClinicalWorks (eCW), one of the leading sellers of record-keeping software for physicians in America, currently used by 850,000 health professionals in the U.S. It didn’t take long for Foster to assemble a dossier of troubling reports — Better Business Bureau complaints, issues flagged on an eCW user board, and legal cases filed around the country — suggesting the company’s technology didn’t work quite the way it said it did. Until this point, Foster, like most Americans, knew next to nothing about electronic medical records, but he was quickly amassing clues that eCW’s software had major problems — some of which put patients, like Annette Monachelli, at risk. Damning evidence came from a whistleblower claim filed in 2011 against the company. Brendan Delaney, a British cop turned EHR expert, was hired in 2010 by New York City to work on the eCW implementation at Rikers Island, a jail complex that then had more than 100,000 inmates. But soon after he was hired, Delaney noticed scores of troubling problems with the system, which became the basis for his lawsuit. The patient medication lists weren’t reliable; prescribed drugs would not show up, while discontinued drugs would appear as current, according to the complaint. The EHR would sometimes display one patient’s medication profile accompanied by the physician’s note for a different patient, making it easy to misdiagnose or prescribe a drug to the wrong individual. Prescriptions, some 30,000 of them in 2010, lacked proper start and stop dates, introducing the opportunity for under- or overmedication. The eCW system did not reliably track lab results, concluded Delaney, who tallied 1,884 tests for which they had never gotten outcomes. The District of Vermont launched an official federal investigation in 2015. The eCW spaghetti code was so buggy that when one glitch got fixed, another would develop, the government found. The user interface offered a few ways to order a lab test or diagnostic image, for example, but not all of them seemed to function. The software would detect and warn users of dangerous drug interactions, but unbeknownst to physicians, the alerts stopped if the drug order was customized. “It would be like if I was driving with the radio on and the windshield wipers going and when I hit the turn signal, the brakes suddenly didn’t work,” said Foster. The eCW system also failed to use the standard drug codes and, in some instances, lab and diagnosis codes as well, the government alleged. The case never got to a jury. In May 2017, eCW paid a $155 million settlement to the government over alleged “false claims” and kickbacks — one physician made tens of thousands of dollars — to clients who promoted its product. Despite the record settlement, the company denied wrongdoing; eCW did not respond to numerous requests for comment. If there is a kicker to this tale, it is this: The U.S. government bankrolled the adoption of this software — and continues to pay for it. Or we should say: You do. Which brings us to the strange, sad, and aggravating story that unfolds below. It is not about one lawsuit or a piece of sloppy technology. Rather, it’s about a trouble-prone industry that intersects, in the most personal way, with every one of our lives. It’s about a $3.7 trillion health care system idling at the crossroads of progress. And it’s about a slew of unintended consequences — the surprising casualties of a big idea whose time had seemingly come. The Virtual Magic Bullet Electronic health records were supposed to do a lot: make medicine safer, bring higher-quality care, empower patients, and yes, even save money. Boosters heralded an age when researchers could harness the big data within to reveal the most effective treatments for disease and sharply reduce medical errors. Patients, in turn, would have truly portable health records, being able to share their medical histories in a flash with doctors and hospitals anywhere in the country — essential when life-and-death decisions are being made in the ER. But 10 years after President Barack Obama signed a law to accelerate the digitization of medical records — with the federal government, so far, sinking $36 billion into the effort — America has little to show for its investment. KHN and Fortune spoke with more than 100 physicians, patients, IT experts and administrators, health policy leaders, attorneys, top government officials and representatives at more than a half-dozen EHR vendors, including
Find Your New Happy Place: WalletHub Releases 2019 “Happiest Cities In America” List

Some travel healthcare professionals already know that where a job is located can have a big impact on how much they enjoy working there. It can be difficult, though, to narrow down which city they will enjoy working in the most. A new list released by WalletHub, a personal finance education website, could help with that issue. WalletHub released the 2019 rankings for their annual “Happiest Cities In America” study Monday, which evaluated 182 of the largest U.S. cities based on 31 indicators of happiness, like the depression rate, income-growth rate and average leisure time spent per day, according to their website. Those key factors were combined into three main categories—”Emotional and Physical Well-Being,” “Income and Employment,” and “Community and Environment,” which produced a composite score for each city. While not all of the indicators listed in the study affect travelers directly—like the rate of separations and divorces in each city—others have a more direct impact, including ideal weather, crime rate, access to parks and open spaces, commute time, and illness and disability rates. The top 10 happiest cities in America, based on WalletHub’s rankings, are: Plano, Texas Irvine, California Madison, Wisconsin Fremont, California Huntington Beach, California Fargo, North Dakota Grand Prarie, Texas San Jose, California Scottsdale, Arizona San Francisco, California Among the top 10, Fremont received the highest rank for “Community and Environment” and San Jose for “Emotional and Physical Well-Being.” Seattle, Washington, which ranked overall at No. 54, received the highest ranking in the “Income and Employment” category. The results are intriguing, but should not be used as the ultimate solution to fixing the blues, experts say. Most studies suggest that finding and fostering happiness is less about a location and more about how people engage with their jobs, their communities and the experiences they choose to have. Travelers can view the full results of the analysis on the WalletHub website.
Travel Jobs: Competition Low, Opportunities High In March As Market Moves Into Spring

The travel healthcare job market is affected by a number of economic and environmental factors, but one of the most prevalent forces shifting job demand are the changes in season. As such, the spring season (and March in particular) represents a major transitional period for the market. Travelers are coming off of winter contracts and are looking for new opportunities in northern states that could turn into summer extensions. One could assume this would mean competition for jobs is fierce in March, but Oren Lavi with LiquidAgents Healthcare said the candidate pool is still slim despite the high number of open positions, meaning jobs are staying open for longer and are easier to book. Since the average length of most travel healthcare job contracts lasts 13 weeks, it’s reasonable to think that most travelers would have just finished their winter contracts from December and are now looking for new opportunities at the start of March. However, many travelers avoid working in December because of the holidays and instead wait until January to start a new contract. This means that, while competition is low for now, travelers can expect to see it ramp up towards the end of March and throughout April. “A lot of nurses need to make extension decisions, and once they do, the market will get flooded with available candidates,” Lavi said. Facilities are most committed to finding qualified candidates that are interested in extending through the summer, so travelers who have already found a breezy and adventurous summer vacation destination up north for their next contract are ahead of the curve. Keep an eye on states like Idaho, Maine, New Hampshire, Oregon, Pennsylvania, Utah and Washington to offer enticing pay packages in March, because they may not stick around as we get closer to summer. Travel Healthcare Jobs March 2019 Here’s a quick breakdown of the states and travel healthcare job specialties that are most-in-demand now and are expected to stay popular in March, according to data provided by staffing industry sales and recruiting representatives. Arkansas RN: Medical-surgical, telemetry, step-down/PCU Surgical Tech: OR, Cath Lab Illinois RN: Medical-surgical, telemetry, step-down/PCU Surgical Tech: OR, Cath Lab Other Notes: Crisis bill rates were recently implemented at OSF HealthCare facilities in Illinois Indiana RN: Medical-surgical, telemetry, ER, ICU. Other Notes: Lots of openings in Indiana right now, but facilities are being more picky with candidates, so jobs are not moving as quickly as they did in February. Kentucky RN: Medical-surgical, telemetry, step-down/PCU Surgical Tech: OR, Cath Lab Maine RN: Medical-surgical, telemetry, ER, ICU. Bill rates up by $10 more than usual on average. Other Notes: Maine is on fire—more than 20 medical-surgical and telemetry nurse needs have been posted in the past two weeks. Hospitals are staffing up for summer break. Nevada RN: Telemetry, OR, CVOR, ICU Surgical Tech: OR Non-Certified Surgical Tech: SPT Other Notes: ER needs are on the decline, but OR and ICU needs are picking up speed. Most positions are coming out of Reno. New Hampshire RN: Medical-surgical, telemetry, ER, ICU. Bill rates have remained high since the start of February. Other Notes: New Hampshire remains a hotspot for ICU needs offering premium bill rates. Oklahoma RN: Medical-surgical, telemetry, ER, ICU Other Notes: Not many job postings available, but when jobs open they close very fast. Quick on callbacks and interviews for qualified candidates. Pennsylvania RN: ICU, OR, medical-surgical, telemetry. Surgical Tech: OR Non-Certified Surgical Tech: SPT Other Notes: Bill rates in Pennsylvania are quite high compared to other states in the region, and have steadily increased in preparation for spring. Texas RN: Medical-surgical, telemetry, step-down/PCU Surgical Tech: OR, Cath Lab
New York, Rhode Island Nursing Unions Vote To Authorize Strikes

Members of registered nurse unions in New York and Rhode Island have both voted to allow union representatives to issue 10-day strike notices if necessary, according to recent reports. United Nurses & Allied Professionals (UNAP) members in Rhode Island voted Wednesday to authorize a strike notice for Fatima Hospital, located in northern Providence. Workers want to bring attention to what they claim is a lack of commitment to patient and worker safety under Prospect CharterCARE, according to a WPRI report. Fatima Hospital is an affiliate of Prospect CharterCARE. “We don’t take this step lightly and we realize what’s at stake for each other, our patients and the community we are proudly a part of,” Cindy Fenchel, president of UNAP Local 5110 said to WPRI. “It’s time for Prospect CharterCARE to come to the table and make substantive commitments on improving patient care and strengthening worker safety.” In New York, more than 8,000 members of the New York State Nurses Association (NYSNA) voted to authorize a 10-day strike notice amid ongoing contract negotiations with New York City Hospital Alliance, according to a recent blog post. The collective bargaining agreement between the two organizations ended on December 31. NewYork-Presbyterian Hospital, Montefiore, Mt. Sinai, Mt. Sinai West, and St. Luke’s hospitals are involved in the negotiations, and a potential strike could affect an estimated 10,000 nurses at those facilities. Nurses held open protests against the 13 facilities in February over what they claim are unsafe working conditions and inadequate staffing levels. New York City Hospital Alliance disputes these claims and said NYSNA has not provided a “single shred of evidence” to support this claim, according to a CBS WLNY report. “We have remained committed to bargaining in good faith and have put forward a significant proposal that demonstrates the value we place on our nurses, who are the best in the business and should be rewarded for their essential role in the delivery of excellent care,” Farrell Sklerov, a spokesperson for the Hospital Alliance told WLNY.
Alabama Legislators Introduce Nursing Compact License Bill

Alabama legislators introduced two bills Tuesday that could allow the state to join the nationwide Nursing Licensure Compact, according to data from Legiscan. House Rep. April Weaver and Sen. Gregg Reed pre-filed and introduced House Bill 44 and Senate Bill 38, respectively, during the first special session of 2019. Both bills were referred to House and Senate health committees for further discussion. If approved, Alabama would become the 32nd state to join the Nursing Licensure Compact, which allows for registered nurses and licensed practical nurses to practice in multiple states without having to apply for a single-state license. It would also allow Alabama nurses easier access to jobs across state lines, as Florida, Georgia, Kentucky, Mississippi and Tennessee are all members of the Nursing Licensure Compact. The Alabama Board of Nursing voiced support for the compact license legislation last Thursday on social media and in their organization’s newsletter, stating that the board decided to pursue the legislation after “very intense, detailed analysis” last September. “This was not an easy decision, as the Board was careful to pay special attention to protecting Alabama’s regulatory prerogatives and to ensure that Compact participation would not negatively impact patient care in the state,” the newsletter statement reads. “The Board is honored to recognize Representative April Weaver, RN (R-Alabaster) and Senator Greg Reed (R-Jasper) for sponsoring the historic bills (House Bill 44 and Senate Bill 38) that would enact the Compact in Alabama. Part of the reason the board wants this legislation to pass is because of the growing nursing shortage in Alabama, according to the statement. Analysts project Alabama will have a surplus of nurses by 2030, according to a 2017 labor study by the Health Resources and Services Administration, but healthcare leaders in the state say they are having problems finding and retaining nurses. Many Alabama healthcare leaders have pointed to common factors affecting the nursing shortage at a national level, including higher demand with an aging population and workforce, a lack of available educators to train more new nurses faster, and issues with pay and working conditions. Alabama is on the lower end for compensation—the average nursing salary in the state is $57,890, according to Bureau of Labor Statistics data. This also includes travel nursing pay, where the average contract ranges from $1,400-1,500 weekly, according to the most recent StaffDNA job board data. Despite this, Alabama remains a fairly popular destination for travelers, and nursing professionals in the state have said travel nursing is also a factor contributing to staff retention issues, according to a WFSA 12 report.
SIA Announces 2019 ‘Best Staffing Firms To Work For’ List

Staffing Industry Analysts announced the winners of their 2019 ‘Best Staffing Firms To Work For’ Wednesday at their 28th annual Executive Forum North America in Austin, Texas, according to a company press release. Among the categories–which were split into eight sections based on company size, types of staffing and geographic location–four U.S. travel healthcare staffing firms took home Grand Prize honors, which are awarded to firms that score the highest in each category. Those four Grand Prize winners from the 2019 Best Staffing Firms To Work For list are: Fusion Medical Staffing (Firms with 201-500 employees) LiquidAgents Healthcare (Firms with 51-200 employees) Health Providers Choice (Firms with 21- 50 employees) Austin Major Group (Firms with 10-20 employees) Each category also had several notable travel healthcare staffing companies that didn’t win a Grand Prize but still placed in the top percentiles of their category, including Atlas Medstaff, Aya Healthcare and Medical Solutions. About 400 staffing agencies participated in the 2019 awards program, which was conducted by SIA in conjunction with Quantum Workplace, according to the press release. Internal employees at each firm were asked to complete a 40-question survey that measured specific quality-of-life and engagement categories, including trust in senior leaders, teamwork, manager effectiveness and more. Staffing firms are not charged for their participation in the awards program and must have a minimum number of employees participate based on their size to ensure statistically sound results, according to the press release. “Congratulations to the winners of this year’s Best Staffing Firm to Work For Awards,” Barry Asin, president of SIA said in a press release. “These high-performing companies stand out for their quality of leadership and as organizations that prioritize culture and employee engagement. There is a strong correlation between employee engagement and growth. These firms have made that connection and use it to excel in their business and drive outstanding results.” Readers can view the full list of winners and top-placing staffing firms here.
‘These Women’s Lives Mattered’: Nurse Builds Database Of Women Murdered By Men (KHN)
By Natalie Schreyer, Kaiser Health News PLANO, Texas — In February 2017, a school nurse in this Dallas suburb began counting women murdered by men. Seated at her desk, beside shelves of cookbooks, novels and books on violence against women, Dawn Wilcox, 55, scours the internet for news stories of women killed by men in the U.S. For dozens of hours each week, she digs through online news reports and obituaries to tell the stories of women killed by lovers, strangers, fathers, sons and stepbrothers, neighbors and tenants. “I’m trying to get the message [across] that women matter, and that these women’s lives mattered, and that this is not acceptable in the greatest country in the world,” Wilcox said. Her spreadsheet, a publicly available resource she calls Women Count USA, is a catalog of lives lost: names, dates, ages, where they lived, pictures of victims and their alleged killers, and the details that can’t be captured by numbers. For Wilcox, these women are more than statistics. She wants you to know Nicole Duckson, a 34-year-old Columbus, Ohio, woman whose friends “remembered her as a prayerful person and a loving mother.” And Duckson’s 4-year-old daughter, Christina, who was stabbed to death alongside her mother, “a polite, happy little girl.” And Claire Elizabeth VanLandingham, 27, a Navy dentist fatally shot by her ex-boyfriend. She had appeared in a video for Take Back the Night, the organization known for fighting dating violence, sexual violence and domestic violence on college campuses nationally. Her mother said, “Her heart was kind; her spirit generous; her soul wise. She gave her smile to everyone who needed it; to everyone who hadn’t even realized they did.” Those are just a few of the nearly 2,500 women listed in Wilcox’s album during the past two years. “Where is the outrage? Where are the marches, the speeches? I know where the silence is. It is everywhere and it is deafening,” Wilcox said. Her crusade, Wilcox said, was spurred in part by the media frenzy about the shooting death of a gorilla, Harambe, at the Cincinnati Zoo and the uproar over the killing of Cecil the Lion, shot by a Minnesota dentist as a trophy. As an animal lover, she was horrified by those killings. But as she saw the social media fury and the online petitions spread, she asked herself: “But what about women?” “Women are people and they deserve to have their lives valued,” she posted on Facebook in 2016 after Harambe’s death. “They deserve our voices speaking out on their behalf. And when they are abused, assaulted, murdered and erased they deserve our attention and our outrage.” Tracking The Data The FBI releases crime data every year, including the number of women who have been killed by men, but local police are not required to file reports to the federal agency, so some state figures are missing. Florida, for example, has not provided its data to the FBI since 1996, according to reports by the Violence Policy Center, a nonprofit organization that advocates to stop gun violence. Numbers from Alabama and Illinois have also been unavailable or limited in certain years. Since 1996, between 1,613 and 2,129 women were murdered by men each year, FBI data show. In 2017, the latest year for which data are available, the FBI counted 1,733 women. An overwhelming majority of those women were killed by a man they knew. “If you just go by the raw numbers, it is undoubtedly an undercount of domestic violence homicides,” said April Zeoli, an associate professor of criminal justice at Michigan State University and an expert on domestic violence homicides and gun laws. Still, she added, “it’s the most accurate picture we have.” Wilcox, however, is doing something the FBI does not: putting faces to the cases. Recording the correct number of women murdered isn’t the only goal of Wilcox’s effort. Her work is about searching for their stories, finding their photos, trying to learn who they were, so that these women aren’t forgotten. Touched By Abuse Wilcox is no stranger to violence against women. When she was 21, she began dating a man she met in a bar in Dallas. She’ll never forget the first time he hurt her. On a night out at a dance club, Wilcox’s boyfriend stepped into the restroom. When he came back, she said, he sprayed cologne into her face, burning her eyes as she groped her way to the bathroom to rinse it out. It was an accident, she said he told her. But Wilcox knew it was an attempt to humiliate her. The violence escalated, Wilcox said, culminating in a night that left a deep scar on the inside of her arm and a memory of abuse that echoes the stories of the lost women for whom she searches. It was hot and the power had gone out, leaving her with no air conditioning as she read a book by candlelight in her apartment. The man began kissing her leg, she said, but soon she felt his teeth digging into her as he bit her. She told him to stop, but he put his hand to the base of her throat, pushed her down onto the bed and, after telling her he wanted to taste her blood, bit into the crook of her arm, tearing out skin, she said. Wilcox went to a hospital emergency room and then fled to her mother’s home. She eventually ended the relationship with the man. He was subsequently convicted of sexual assault and kidnapping after he raped two women before forcing them into his car, driving them to a secluded, wooded area, knocking them out and threatening to kill them. The women managed to escape. Wilcox considers herself lucky. “I could’ve easily ended up one of the women on my own list.” Today, she is married to a man who said his wife’s work has opened his eyes to the pervasiveness of violence against women. “She’s inspired me,” said Mike Nosenzo,
