Traveler Tips: How to Handle Bullying as a Travel Nurse

By Alex McCoy, Contributing Writer, Owner of Fit Travel Life Last week I discussed how travel nurses may encounter bullying on the job. This type of lateral violence may present differently when you work as a traveler than when you are permanent staff. Ready for the good news? This also means as a traveler you have other ways to handle nurse bullying to keep yourself safe and happy. While working as a temporary staff member may open us up to more scrutinization than other scenarios, it also gives us some very powerful advantages we can use to make our situation better for ourselves. Here are a few ways I have handled assignments where the staff has felt less than welcoming. Don’t get caught up in gossip. I have found that units that have higher rates of gossip among staff also tend to have higher rates of nitpicking and hurt feelings. It only takes a couple of days on a floor to gauge whether there is a high or low rate of chatter behind backs. If I sense there is a lot of gossip going on, I purposely remove myself from these conversations because the last thing I want to do is upset a new coworker by giving the impression that I am in the wrong social circle. We are not obligated to make friends with other staff members at each new assignment, so we have the advantage of simply coming to work for our patients and leaving personal relationships at the door. Similarly, I have found myself chatting with other travelers who turn out to be very negative or outspoken about the facility and staff. In these situations, I make a point to distance myself from that person, and if we end up working together regularly I try to shut down the negativity as fast as possible. Keeping a middle ground on opinions about an assignment can be very helpful in staying out of the drama. Focus on your days off rather than your work days. In some situations, we simply cannot change the work environment we are walking into. If the unit I am working on is not only physically but emotionally draining I shift to a “get in, get out” mindset. While picking up extra shifts or staying late for overtime can be tempting, there is nothing worth sacrificing your mental health to an unfriendly environment for longer than necessary. During stressful assignments, I also make a point to practice purposeful self-care on my off days. I prioritize exercise, rest, and getting some sunshine because those are the things I know make me happy. One assignment may require a little more downtime than the next, so be sure to read your body’s cues and listen to what it needs on your days off. Embrace the “It’s only 13 weeks” mindset. It can be easy to get caught up in drama or rude staff behaviors, but the beauty of travel is we get to walk away at the end of our assignment no matter what. It might sound a little selfish, but if I find myself feeling particularly irritated by a staff member, I take the time to think about how at the end of 13 weeks I get the option to move on to better opportunities while they are stuck in a job that is not serving them well. Of course, these thoughts are probably best kept to yourself or expressed to a close friend, but sometimes just getting your feelings out can make a world of difference. Don’t be afraid to report and document mistreatment. As travel nurses, we have an extra layer of protection that comes from our company. While I don’t advise running to your recruiter for every small issue they can be helpful in navigating particularly unprofessional encounters. I typically keep my recruiter in the loop if I anticipate a situation could get worse, so I have documentation from the very beginning. If you are in a situation where you are feeling depressed, anxious, or fearful about returning to work due to bullying, reach out to your travel company and ask to speak to their clinical liaison. This is someone who has worked in healthcare and is experienced in navigating tough professional situations. Most companies are also thankful to know of situations that are less than ideal for their travelers so they can possibly avoid future placements at facilities that do not treat temporary staff well. At the end of the day, being prepared mentally will serve you well. Lateral violence is not something we should have to deal with, but unfortunately, most experienced nurses have encountered it at some point in time. Going in with tools to approach these situations can be helpful in keeping yourself sane through a more difficult assignment. Each assignment will bring with it a different culture to navigate. I am happy to say that my experience as a travel nurse has been overwhelmingly positive, and most staff is thrilled to have the extra helping hands. The naysayers are few and far between, and having these mental practices in place has helped tremendously with focusing on the positives of each assignment rather than the negatives. Alex McCoy currently works as a pediatric travel nurse. She has a passion for health and fitness, which led her to start Fit Travel Life in 2016. She travels with her husband, their cat, Autumn and their dog, Summer. She enjoys hiking, lifting weights, and trying the best local coffee and wine. << Part One: Types of Bullying Travelers Encounter
Enhanced Nurse Licensure Compact Now Effective in Kansas and Louisiana
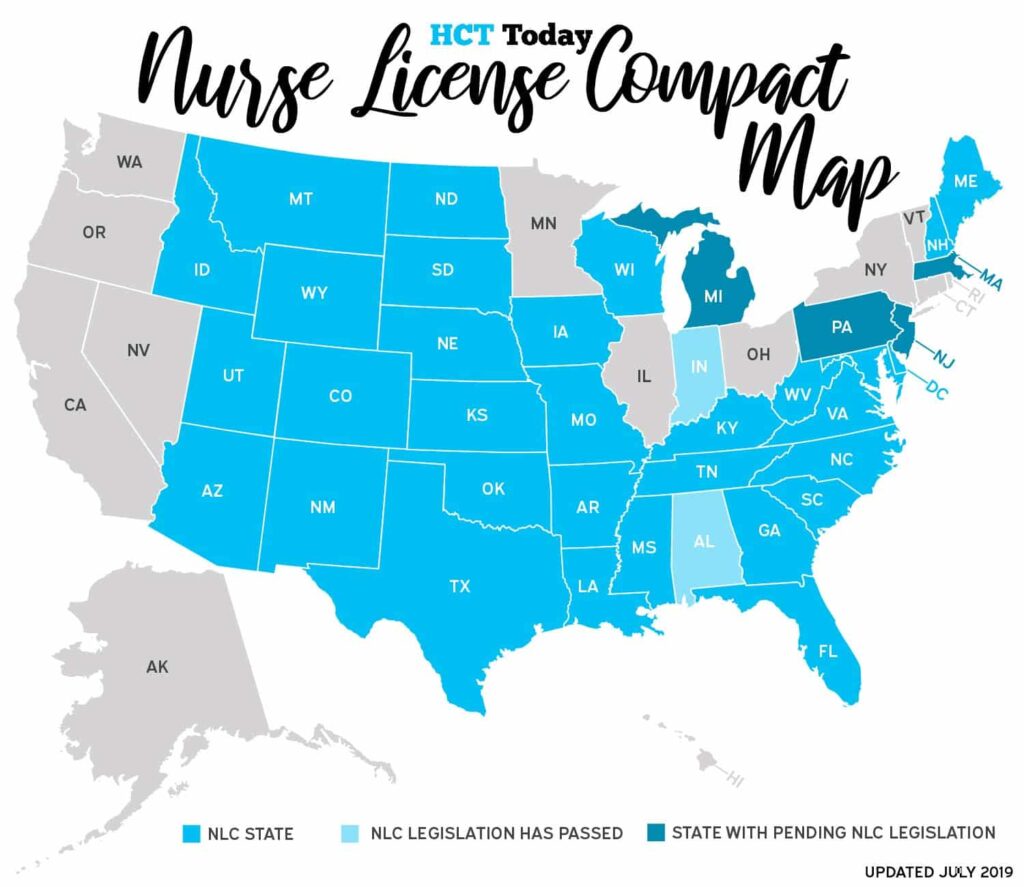
After much anticipation, the Enhanced Nurse Licensure Compact (eNLC) is now in full operation in Kansas and Louisiana effective today, July 1. Starting immediately, travel nurses with a compact license can practice in these two new states. Additionally, resident RNs and LPNs can apply for a compact license, which gives them access to practice in all 31 compact states. This helps open up the healthcare travel market, benefiting both these states and allowing more nurses to easily practice across state lines. Legislation to join the eNLC was passed in April 2018 for Kansas and June 2018 for Louisiana. Alabama and Indiana are up next. Alabama is anticipating full implantation by January 1, 2020, while Indiana’s target date is undetermined. Current states with pending legislation to join the eNLC include Pennsylvania, New Jersey, Michigan and Massachusetts. To apply for a compact license, find your respective state board of nursing HERE. Related article: New Jersey Compact Nursing License Passes, Sent to Governor for Final Signature
Traveler Tips: Types of Bullying Travelers Encounter
By Alex McCoy, Contributing Writer, Owner of Fit Travel Life I’m not sure exactly when I first heard the phrase “nurses eat their young” but I know it was very early on in my nursing career. In fact, I am almost positive I heard it from a nursing professor before I had even set foot on a hospital floor. This unfortunate culture is one that has been brought to the forefront of healthcare related news more and more lately, and I do believe there is a strong wave of nurses working to put an end to this stereotype. However, each unit and hospital across the country has different people and practices that may contribute to this outdated culture and it is something we have to be prepared to deal with as travelers. The term “bullying” is broad. This can refer to many different negative behaviors and ultimately it boils down to how the person being treated feels about their treatment. What one individual can overlook may totally ruin an assignment for someone else, so it is important to be aware of the different forms bullying can take so we can better intervene or support other nurses when we see it happening. Here are a few types of bullying I have witnessed as staff and as a traveler. Overanalyzing how someone performs a task. In the medical field, there are about 100 ways to do the same tasks. For example, in some places, it is unheard of to prime blood tubing without first priming with saline, and in other places, it is standard practice to hang the blood first. Regardless of your personal opinions, different hospitals have research committees that sit down and write policies that may be at odds with each other but at the end of the day are meant to have the patients’ best interests in mind. A quick way to make a nurse feel unwelcome is to comment directly on how he or she performs a specific task without asking why they did it that way. The more frequently this happens, the more self-conscious or frustrated that nurse may become. I have had nurses look at me like I have three heads when I do something a certain way when it was common practice at my previous three assignments. Approach these instances from a place of wanting to learn rather than criticizing and you may find a better way to perform your job in the long run. Intentional exclusion. As the newbie on a unit, I by no means expect to be included in every conversation or event, but I do think it is hurtful when everyone except the traveler(s) are invited. There is a very awkward moment when you realize the conversation shuts down when you come around, and it makes adjusting to a new unit that much more uncomfortable. While it can be hard to get to know someone during a shift, it is even harder if you are unwilling to try to know them outside of work. If there is a group of people going to drinks after work or to a festival on the weekend, keep in mind that purposely excluding the new kid can be more harmful than you realize, especially if you haven’t been that newbie in a long time. Micromanaging tasks and charting. Each assignment comes with a 2-3 week adjustment period where I welcome [helpful] feedback or tips on how certain situations are handled at each particular job. Some facilities are very task-oriented, others have policies outlined for every scenario, and some are more go with the flow. As I get a handle on these things it can be helpful to have a few tips or tricks given to me by full-time staff members of how to best manage my day or keep on top of what is most important on that particular unit. What is not helpful is coming on to a shift to find an email or laundry list of things I did “wrong”. The majority of travelers know the basics of being a nurse very well, they just need a little guidance in unit specifics. A small hiccup or forgotten piece of charting doesn’t mean the nurse is incompetent, it may just mean that is not something they have had to chart or focus on previously. However, being the victim of constant nitpicking or feeling like your charting is being double-checked constantly can be very mentally draining on a traveler. Most travelers go in with one of two mindsets. Either they assume the staff at their new job will be so overjoyed to have the help that they will be over the top nice, or they hear horror stories about nurse bullying and go in with their guard up from the beginning. Personally, I have found that approaching each assignment with an open mind has led to a better overall experience, but after seeing how some staff behave toward travelers I can see how some nurses can come in with the latter attitude. Next week I will cover exactly how to handle negative behavior while on assignment, including some advantages that we as travelers have that full-time staff do not. While this should not be a part of nursing (or any job) it is an unfortunate truth we have to be ready to handle with grace in order to keep our own morale up in order to keep enjoying all the perks that travel nursing has to offer. Alex McCoy currently works as a pediatric travel nurse. She has a passion for health and fitness, which led her to start Fit Travel Life in 2016. She travels with her husband, their cat, Autumn and their dog, Summer. She enjoys hiking, lifting weights, and trying the best local coffee and wine. << Part Two: How to Handle Bullying as a Travel Nurse
Traveler Tips: Eating Healthy on Road Trips

By Alex McCoy, Contributing Writer, Owner of Fit Travel Life I’m sure by now a lot of people have seen the meme floating around that says “Shopping for road trip snacks should always look like an 8-year-old set loose in a convenience store” (probably not a direct quote, but you get the idea). And while this may be true for those once-in-a-lifetime road trips with your bestie, a healthcare traveler’s road trip schedule is usually a little different. For those of us who drive back and forth across the country several times per year, this style of road trip eats is not a very healthy or sustainable way to live. Not only do we spend a lot of time in the car between assignments, but many of our days off are spent driving to the nearest well-known attraction in our area. If we spent every moment in the car chowing down on Doritos and gummy worms, we’d likely end up ten pounds heavier at the end of each assignment. While it isn’t always easy to eat healthy on these long treks, it can be done. Here are a few of my best tips for keeping your nutrition in check while spending hours in the car. 1. Go in with the right mindset. If long term health is your goal, keep that in mind when you set off on your trip. Rather than approaching your drive with the mindset “I am on the road so I’ll just have to do better when I get there” try thinking “What small choices can I make so I feel better at the end of this trip?” The reality for most of us is we can’t prep and pack our meals for these trips, but we can control small choices we make over the course of several days. Remember that you don’t have to be perfect and convenience will be necessary, but that doesn’t mean it’s time to binge or completely disregard healthy choices. 2. Don’t drink your calories. On road trips, I drink two beverages: coffee and water. If I stop somewhere like Starbucks, I only get skim milk or sugar-free syrups added to my coffee to keep the sugar and fat content low. If I get bored with water, I may add a Crystal Lite packet or grab a sparkling water, but overall I stick to plain water in a reusable cup. If plain coffee is a total no-go for you, check out the Macro Barista on Instagram. He posts tons of great recipes and how to order them at Starbucks 3. Pick one snack at each stop. Especially if you are driving late at night, it can be difficult to avoid snacking completely while driving. Rather than loading up on three or four options, I pick one snack (usually salty fair) and try to stretch it out until the next stop. Some of my favorites that I have found at most travel centers are Skinnypop, Pop Chips, or even plain popcorn if I can’t find anything else. If you are more into sugary snacks, try to pick the smallest portion or portion out a small handful and put the rest of the package away. It can be so easy to absentmindedly eat a whole bag of candy while you are busy driving, so plan ahead to keep yourself from accidentally doing this. 4. Strategically plan your stops. When you sit down and plan your drive for the day, make a rough plan of where the best places will be to stop for larger meals. I know I will be hungry every three to four hours, so if I hit a larger town with more options around the three-hour mark, I know it is probably better to just stop then because it may be a while before I hit another place with multiple places to eat a meal. Just to note–I essentially never sit down and eat. When mealtime rolls around I make a mental list of places that sound good, and as soon as I see one of those places I stop. There is nothing worse than waiting for a particular option than getting to the end of a city and realizing there are no more places to eat. 5. Have a list of “better” fast food options. Anyone who has road tripped for longer than five or six hours could probably list the top five restaurants you see most frequently at rest stops. These options are pretty basic especially when traveling through rural parts of the country. I have a small list of entrees at most of these places that do not consume an entire day’s worth of calories and I stick to these options when we stop. On road trips, I am typically eating fast food out of necessity, not because I am truly craving something specific, so I just eat what I know is best for me and move about my day. While road trip eats won’t always be the most wholesome, the good news is many chains and fast food restaurants have shifted to have at least one or two options that are better than their standard fare. Focus on the things you can control and be mindful of your water intake. At the end of the day, these small choices will add up over time, and leave you feeling much better than spending three days in a car downing bags of salty food and slamming energy drinks. Alex McCoy currently works as a pediatric travel nurse. She has a passion for health and fitness, which led her to start Fit Travel Life in 2016. She travels with her husband, their cat, Autumn and their dog, Summer. She enjoys hiking, lifting weights, and trying the best local coffee and wine.
Are Metro Areas Taking Rural Hospitals’ Travel Nurses?

Traditionally, travel nursing is known for helping rural hospitals thrive. Example: A less than 50-bed hospital in a remote town, hours from any large urban setting is unable to attract and retain long-term staff; so the facility relies heavily on healthcare travelers to bring skilled, quality care to the community. Travel nurses and allied professionals are typically offered better pay, benefits and flexibility at more rural facilities than they would get at home. But looking at recent trends in today’s travel healthcare market, rural facilities are being faced with more competition from metropolitan areas. A recent study by Navigant Healthcare reported 21 percent of rural hospitals nationwide are at high risk of closing, which includes 34 states that have five or more facilities at a great risk. Top states include Alabama, Mississippi, Georgia, Maine, Alaska, Arkansas, Oklahoma, Kansas, Michigan, Kentucky, Minnesota and Iowa. Alabama tops the list with the highest percentage of rural facilities most at risk, totaling 50 percent in the state. Chief policy officer at the Alabama Hospital Association Danne Howard recently shared with Modern Healthcare that this is “probably the most fragile of situations I have seen in my 23 years at the association.” Georgia follows close behind with 41 percent of the state’s rural facilities facing high risk of closure. Last week, the Augusta Free Press reported that Georgia is facing one of the worst nursing shortages in the country. According to the article, some resources are forecasting that by 2030, Georgia will be short up to 50,000 nurses needed to provide proper patient care. The healthcare staffing openings on the StaffDNA Job Board align with these reports, and it’s not only rural areas in need of travel healthcare professionals. Georgia’s two most populated cities, Atlanta and Augusta, have the state’s most openings for travel nurses and allied professionals on the StaffDNA Job Board. Depending on the specialty, travel RN positions in Georgia’s metro areas are offering similar to or even higher pay rates than the rural facilities. More than ever before, rural hospitals are competing with larger cities to attract healthcare professionals. This trend can be seen across the country. But being in a rural area doesn’t mean the patient pool decreases. Healthcare travelers are and will continue to be a driving force to keep rural facilities running and able to provide quality care in their communities. How are rural hospitals attracting travelers? Community. At rural facilities, travel nurses are treated like family, both in the hospital and out in the community. In a small-town setting, hiring managers look for travelers who are adaptable, and can understand and appreciate the local culture. Nurses and allied health professionals have their own reasons for traveling—experience new locations, pay off debt, build resume, avoid hospital politics, etc.—but one focus remains the same: patient care. Whether it’s a small rural facility or Level 1 trauma center in the heart of the city, healthcare travelers are making positive impacts in every community they serve. Read Next: How to Set Realistic Expectations for Your Healthcare Travel Career
Escalating Workplace Violence Rocks Hospitals (KHN)

Marlene Harris-Taylor, Ideastream Across the country, many doctors, nurses and other health care workers have remained silent about what is being called an epidemic of violence against them. The violent outbursts come from patients and patients’ families. And for years, it has been considered part of the job. When you visit the Cleveland Clinic emergency department — whether as a patient, family member or friend — a large sign directs you toward a metal detector. An officer inspects all bags and then instructs you to walk through the metal detector. In some cases, a metal wand is used — even on patients who come in on stretchers. Cleveland Clinic officials say they confiscate thousands of weapons like knives, pepper spray and guns each year. The metal detectors were installed in response to what CEO Tom Mihaljevic calls an epidemic. “There is a very fundamental problem in U.S. health care that very few people speak about,” he said, “and that’s the violence against health care workers. Daily — literally, daily — we are exposed to violent outbursts, in particular in emergency rooms.” Many health care workers say the physical and verbal abuse come primarily from patients, some of whom are disoriented because of illness or from medication. Sometimes nurses and doctors are abused by family members who are on edge because their loved one is so ill. Cleveland Clinic has introduced other safety measures — such as wireless panic buttons incorporated into ID badges and more safety cameras and plainclothes officers in ERs. But these incidents aren’t limited to emergency rooms. Allysha Shin works as a registered nurse in neuroscience intensive care at the University of Southern California’s Keck Hospital in Los Angeles. One of the most violent incidents she has experienced happened when she was caring for a patient who was bleeding inside her brain. The woman had already lashed out at other staff, so she had been tied to the bed, Shin said. She broke free of the restraints and then kicked and punched Shin in the chest — before throwing a punch at her face. “There was this one point where she swung, and she had just glanced off the side of my chin. If I hadn’t dodged that punch, she could have knocked me out,” Shin said. “And she very well could have killed me.” The encounter left Shin shaken and anxious when she returned to work days later. She still has flashbacks. She used to be afraid to speak about these types of attacks, she said, because of what she calls a culture of accepting violence in most hospitals. “It is expected that you are going to get beat up from time to time,” Shin said. According to the Occupational Safety and Health Administration, incidents of serious workplace violence are four times more common in health care than in private industry. And a poll conducted by the American College of Emergency Physicians in August found nearly half of emergency physician respondents reported having been physically assaulted. More than 60% of them said the assault occurred within the previous year. Groups representing doctors and nurses say that, while the voluntary safety improvements that some hospitals have enacted are a good first step, more needs to be done. There is still a code of silence in health care, said Michelle Mahon, a representative of the labor group National Nurses United. “What happens if they do report it?” she said. “In some cases, unfortunately, they are treated as if they are the ones who don’t know how to do their job. Or that it’s their fault that this happened.” “There’s a lot of focus on de-escalation techniques,” Mahon added. “Those are helpful tools, but oftentimes they are used to blame workers.” In California, the nurses’ labor union pushed for a law giving OSHA more authority to monitor hospital safety. The group is now backing a national effort to do the same thing. “The standard that we are recommending federally holds the employer responsible,” Mahon said. “It mandates reporting of incidents and transparency.” The Workplace Violence Prevention for Health Care and Social Service Workers Act, introduced last fall in Congress, would require hospitals to implement plans to prevent violence. And any hospital could face fines for not reporting incidents to OSHA, Mahon said. The goal of the legislation — and of the union — is to hold administrators more accountable for acts of violence in their hospitals. >> Up Next: ‘John Doe’ Patients Sometimes Forces Hospital Staff to Play Detective This story is part of a partnership that includes Ideastream, NPR and Kaiser Health News. Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
Travel Nursing Stories: My Favorite Parts About Living In Arizona

By Alex McCoy, Contributing Writer, Owner of Fit Travel Life When people ask me what my favorite travel nurse assignment location has been so far, I always tell them Phoenix. We have now been lucky enough to spend two winters in the southwest and do not regret circling back to this location one bit. From hiking to good food to national treasures, there is an abundance of activities to keep you busy no matter what the season. Even as it begins to heat up, we have still found plenty to do, and even joked that Phoenix would be the one place we may have considered settling down permanently. Here are just a few reasons we really love this area of the country. You can experience a variety of climates within a short distance. While Phoenix winter can’t be beat (75 and sunny 95% of the time–what could go wrong?) it does get pretty toasty during the summer, with temperatures already creeping into the double digits in mid-May. However, just take a short trip up to Flagstaff or Sedona (about two hours away) and you will find temperatures are back to a much more comfortable range. In the winter months, you can even head that direction for skiing and other cold-weather fun if that’s your thing. We love the fact that we’ve been able to take a break from warm weather one day then go back to soaking in the pool the next day. There are trails galore–even in the cities. While a lot of states are known for hiking, Arizona is particularly impressive in that you do not have to drive all that far to experience some awesome hiking. In Phoenix alone there is South Mountain Park, Camelback Mountain, and Piestewa Peak in the actual city limits. Take a drive down any major highway and you will find that there are opportunities to get out and explore in just about any direction. From the Painted Desert to the Superstition Wilderness to Grand Canyon National Park, no matter which area of the state you visit you will have no problem finding somewhere to get out and move. There are a ton of delicious local restaurants. Some of the best food I have ever eaten has been during our times in Phoenix. Of course you can find amazing Mexican food and margaritas, but the culinary experiences don’t end with the delicious Mexican food. Simply look at the list for the Arizona Restaurant Week coming up and you will see that just about any palate can be satisfied by the local fare in the area. On our trip to Tucson, we were pleasantly surprised to find that the neighboring city followed this trend. While I expected there to be a variety of food as in any big city, I have been blown away by the quality of just about every place we have eaten on our nights out. It is an easy drive to a lot of fun cities and attractions. Some of the best photo ops in the country can be found in the state of Arizona. Antelope Canyon, Horseshoe Bend and the Grand Canyon are within an hour or so of each other. Zion National Park is just across the Arizona-Colorado border. The beautiful falls of Havasupai are also close (if you can snag a permit) and this doesn’t even touch on all of the scenery in some of the protected areas like the Tonto National Forest. And if you aren’t big into the outdoors, San Diego or Las Vegas are also a quick weekend trip away. Whether you are craving sunshine, beach life or some gambling time, Arizona is a great centrally located spot to mix up your entertainment on your days off. The people are friendly. While Phoenix and Tucson have a lot of the perks of big cities, the people there haven’t shifted into the larger city coolness I have experienced in other large cities. My husband and I have thoroughly enjoyed our coworkers while living in Arizona, and have also found it easy to make friends both at work and outside of work. We have been lucky enough to stay pretty busy with our social lives and have been active in our gym, met coworkers for evenings out, and joined sports leagues while we were here with ease. As a travel nurse, living away from familiar faces can be tough so it’s always nice to live in an area with people who are willing to embrace the newbies as they come along. My biggest takeaway is don’t let the heat or desert life scare you away. Living in Arizona has shown me that there is so much more to the southwest than cacti and sand. The landscape is actually quite varied and beautiful, there are a variety of climates to experience, and the food can’t be beat. Whether you are looking for a fun, thriving vibe in a travel location or a great place to connect with the outdoors, Arizona has something to offer you. You will stay busy on your days off and feel welcomed by staff, which are two things we have greatly appreciated during our time here. Alex McCoy currently works as a pediatric travel nurse. She has a passion for health and fitness, which led her to start Fit Travel Life in 2016. She travels with her husband, their cat, Autumn and their dog, Summer. She enjoys hiking, lifting weights, and trying the best local coffee and wine. Find your next high-paying assignment in Arizona!
Modern Healthcare Recognizes Staffing Agencies In ‘Best Places To Work’ 2019 List

Modern Healthcare, an organization that focuses on healthcare business news, analytics, research and data, released their annual ‘Best Places To Work in Healthcare’ awards list last Saturday, and several travel nursing and allied healthcare staffing agencies were named among the winners. The ‘Best Places To Work’ awards seek to identify and recognize outstanding healthcare employers on a national level, according to their website. Companies that choose to participate for the award are selected for the list through confidential employee surveys. The surveys measure key factors to success, like work-life balance, benefits and employee satisfaction. “Organizations making this year’s list of ‘Best Places to Work in Healthcare’ stand out in their efforts to create an empowered and satisfied workforce,” Modern Healthcare said in a recent post. “They did so by nurturing a sense of loyalty and building engagement.” The alphabetical list released recognizes 150 healthcare companies, and the official rankings will be released on September 26 at the Best Places To Work in Healthcare Gala. They will also be featured in a supplement published with Modern Healthcare’s Sept. 30 issue, according to the post. Among the winners, travel staffing agencies LiquidAgents Healthcare and Aya Healthcare are both repeat honorees. This marks the 11th year in a row that LiquidAgents Healthcare, based out of Plano, Texas, has been recognized as a ‘Best Place to Work’, according to their company press release. “It’s an honor to be recognized among the nation’s top healthcare companies to work for in the country,” LiquidAgents Healthcare CEO Sheldon Arora said in a press release. “We’ve established a unique, collaborative culture with a key focus in mind: to help employees be as successful as possible in their roles and careers. Our team’s positivity and dedication shine through in everything we do.” Aya Healthcare made the list for the third consecutive year, according to a company press release. President and CEO Alan Braynin said the recognition highlight’s Aya’s focus in providing an engaging and exciting workplace. “This recognition is a testament to our belief that giving employees freedom, flexibility and a voice is beneficial for the entire company, including the clinicians and clients we serve,” Braynin said in the release. Other staffing agencies that made the 2019 list include CHG Healthcare, MPLT Healthcare, and several other non-travel specific staffing companies. The full list can be viewed below or on the Modern Healthcare website. COMPANY LOCATION Abrom Kaplan Memorial Hospital Kaplan, La. American College of Cardiology Washington, D.C. Atlantic Health System Morristown, N.J. Bailey Medical Center Owasso, Okla. Beach Cities Health District Redondo Beach, Calif. Black River Memorial Hospital Black River Falls, Wis. Bridge Connector Nashville CAQH Washington, D.C. CareSource Dayton, Ohio Carolina Caring Newton, N.C. Catholic Health Services of Long Island Centre, N.Y. CHG Healthcare Midvale, Utah Choice Recovery Columbus, Ohio Cleveland Clinic Cleveland CollaborateMD Orlando, Fla. Conway Regional Health System Conway, Ark. Corazon Pittsburgh Cox Monett Hospital Monett, Mo. Crothall Healthcare Wayne, Pa. Deaconess-The Women’s Hospital Newburgh, Ind. Divurgent Virginia Beach, Va. Elevate Healthcare Consultants Plano, Texas Encompass Health – Home Health & Hospice Dallas Epion Health Hoboken, N.J. Equiscript North Charleston, S.C. Excel Health Philadelphia Forcura Jacksonville, Fla. Galen Healthcare Solutions Chicago Guadalupe Regional Medical Center Seguin, Texas Harmony Healthcare IT South Bend, Ind. Health By Design Medical Group San Antonio Health Catalyst Salt Lake City Health Recovery Solutions Hoboken, N.J. HealthFirst TPA Tyler, Texas HealthRise Southfield, Mich. Heart Care Imaging Tequesta, Fla. Heart ‘n Home Hospice Fruitland, Idaho Hendrick Health System Abilene, Texas Henry County Hospital Napoleon, Ohio Hillcrest Hospital Cushing Cushing, Okla. Hillcrest Hospital Henryetta Henryetta, Okla. Hillcrest Hospital Pryor Pryor, Okla. Hosparus Health Louisville, Ky. IEP (Independent Emergency Physicians) Farmington Hills, Mich. Impact Advisors Naperville, Ill. Imprivata Lexington, Mass. Infusion Express Brentwood, Tenn. Innovative Health Scottsdale, Ariz. Intelligent InSites West Fargo, N.D. J2 Interactive Charlestown, Mass. Jackson Physician Search Alpharetta, Ga. Jamestown Regional Medical Center Jamestown, N.D. Jellyfish Health Panama City, Fla. KeyBridge Medical Revenue Care Lima, Ohio King’s Daughters Medical Center Brookhaven, Miss. Landmark Health Huntington Beach, Calif. Lee’s Summit Medical Center Lee’s Summit, Mo. Lexington Regional Health Center Lexington, Neb. Licking Memorial Health Systems Newark, Ohio LiquidAgents Healthcare Plano, Texas LiveData Cambridge, Mass. Loma Linda University Medical Center-Surgical Hospital San Bernardino, Calif. Louisiana Organ Procurement Agency Covington Lovelace UNM Rehabilitation Hospital Albuquerque Lovelace Women’s Hospital Albuquerque Marathon Health Winooski, Vt. Medasource Royal Oak, Mich. Medical Advantage Group Ann Arbor, Mich. Medpricer Walnut Creek, Calif. Melissa Memorial Hospital Holyoke, Colo. Memorial Healthcare System Hollywood, Fla. Mercy Health-Tiffin Hospital Tiffin, Ohio Mercy Health-Willard Hospital Willard, Ohio Methodist Ambulatory Surgery Hospital San Antonio Metrolina Nephrology Associates Charlotte, N.C. Morrison Healthcare Sandy Springs, Ga. MPLT Healthcare Coral Springs, Fla. MTS Physical Therapy & Wellness Lafayette, La. Nathan Adelson Hospice Las Vegas National Medical Billing Services St. Louis Navin, Haffty & Associates Westborough, Mass. NCCPA (National Commission on Certification of Physician Assistants) Johns Creek, Ga. Neosho Memorial Regional Medical Center Chanute, Kan. Nova Healthcare Administrators Buffalo, N.Y. Pacific Companies Aliso Viejo, Calif. Parkview Huntington Hospital Huntington, Ind. Parkview LaGrange Hospital LaGrange, Ind. Parkview Noble Hospital Kendallville, Ind. Parkview Wabash Hospital Wabash, Ind. Parkview Whitley/Warsaw Hospital Columbia City, Ind. Pelham Medical Center Greer, S.C. Physicians Surgical Hospitals Amarillo, Texas Propeller Health Madison, Wis. Providence Holy Cross Medical Center Mission Hills, Calif. Providence Little Company of Mary Medical Center Torrance, Calif. Rendina Healthcare Real Estate Jupiter, Fla. Rio Grande Regional Hospital McAllen, Texas RiverView Health Crookston, Minn. Santa Rosa Consulting Franklin, Tenn. Seton Medical Center Harker Heights Harker Heights, Texas Shriners Hospitals for Children-Erie Erie, Pa. Signature Performance Omaha, Neb. Southern Tennessee Regional Health System-Pulaski Pulaski St. Bernards Medical Center Jonesboro, Ark. Stillwater Medical Center Stillwater, Okla. Sutter Amador Hospital Jackson, Calif. Sutter Roseville Medical Center Roseville, Calif. Tandigm Health West Conshohocken, Pa. TigerConnect Santa Monica, Calif. Tri-Cities Cancer Center Kennewick, Wash. TSI Healthcare Chapel Hill, N.C. Tulsa Spine & Specialty Hospital Tulsa, Okla. University Hospital & Clinics Lafayette, La. Uvalde Memorial Hospital Uvalde, Texas Wallowa County Health Care District Enterprise, Ore. Weber Human Services Ogden, Utah
‘John Doe’ Patients Sometimes Force Hospital Staff To Play Detective (KHN)

By Susan Abram and Heidi de Marco, Kaiser Health News The 50-something man with a shaved head and brown eyes was unresponsive when the paramedics wheeled him into the emergency room. His pockets were empty: no wallet, no cellphone, not a single scrap of paper that might reveal his identity to the nurses and doctors working to save his life. His body lacked any distinguishing scars or tattoos. Almost two years after he was hit by a car on busy Santa Monica Boulevard in January 2017 and transported to Los Angeles County+USC Medical Center with a devastating brain injury, no one had come looking for him or reported him missing. The man died in the hospital, still a John Doe. Hospital staffs sometimes must play detective when an unidentified patient arrives for care. Establishing identity helps avoid the treatment risks that come with not knowing a patient’s medical history. And they strive to find next of kin to help make medical decisions. “We’re looking for a surrogate decision-maker, a person who can help us,” said Jan Crary, supervising clinical social worker at L.A. County+USC, whose team is frequently called on to identify unidentified patients. The hospital also needs a name to collect payment from private insurance or government health programs such as Medicaid or Medicare. But federal privacy laws can make uncovering a patient’s identity challenging for staff members at hospitals nationwide. At L.A. County+USC, social workers pick through personal bags and clothing, scroll through cellphones that are not password-protected for names and numbers of family or friends, and scour receipts or crumpled pieces of paper for any trace of a patient’s identity. They quiz the paramedics who brought in the patient or the dispatchers who took the call. They also make note of any tattoos and piercings, and even try to track down dental records. It’s more difficult to check fingerprints, because that’s done through law enforcement, which will get involved only if the case has a criminal aspect, Crary said. Unidentified patients are often pedestrians or cyclists who left their IDs at home and were struck by vehicles, said Crary. They might also be people with severe cognitive impairment, such as Alzheimer’s, patients in a psychotic state or drug users who have overdosed. The hardest patients to identify are ones who are socially isolated, including homeless people — whose admissions to hospitals have grown sharply in recent years. In the past three years, the number of patients who arrived unidentified at L.A. County+USC ticked up from 1,131 in 2016 to 1,176 in 2018, according to data provided by the hospital. If a patient remains unidentified for too long, the staff at the hospital will make up an ID, usually beginning with the letter “M” or “F” for gender, followed by a number and a random name, Crary said. Jan Crary, supervising clinical social worker at Los Angeles County+USC Medical Center, leads a team who increasingly must play detective when patients cannot be identified. Other hospitals resort to similar tactics to ease billing and treatment. In Nevada, hospitals have an electronic system that assigns unidentified patients a “trauma alias,” said Christopher Lake, executive director of community resilience at the Nevada Hospital Association. The deadly mass shooting at a Las Vegas concert in October 2017 presented a challenge for local hospitals who sought to identify the victims. Most concertgoers were wearing wristbands with scannable chips that contained their names and credit card numbers so they could buy beer and souvenirs. On the night of the shooting, the final day of a three-day event, many patrons were so comfortable with the wristbands that they carried no wallets or purses. More than 800 people were injured that night and rushed to numerous hospitals, none of which were equipped with the devices to scan the wristbands. Staff at the hospitals worked to identify patients by their tattoos, scars or other distinguishing features, as well as photographs on social media, said Lake. But it was a struggle, especially for smaller hospitals, he said. The Health Insurance Portability and Accountability Act (HIPAA), a federal law intended to ensure the privacy of personal medical data, can sometimes make an identification more arduous because a hospital may not want to release information on unidentified patients to people inquiring about missing persons. In 2016, a man with Alzheimer’s disease was admitted to a New York hospital through the emergency department as an unidentified patient and assigned the name “Trauma XXX.” Police and family members inquired about him at the hospital several times but were told he was not there. After a week — during which hundreds of friends, family members and law enforcement officials searched for the man — a doctor who worked at the hospital saw a news story about him on television and realized he was the unidentified patient. Hospital officials later told the man’s son that because he had not explicitly asked for “Trauma XXX,” they could not give him information that might have helped him identify his father. Prompted by that mix-up, the New York State Missing Persons Clearinghouse drafted a set of guidelines for hospital administrators who receive information requests about missing persons from police or family members. The guidelines include about two dozen steps for hospitals to follow, including notifying the front desk, entering detailed physical descriptions into a database, taking DNA samples and monitoring emails and faxes about missing persons. California guidelines stipulate that if a patient is unidentified and cognitively incapacitated, “the hospital may disclose only the minimum necessary information that is directly relevant to locating a patient’s next-of-kin, if doing so is in the best interest of the patient.” At L.A. County+USC, most John Does are quickly identified: They either regain consciousness or, as in a majority of cases, friends or relatives call asking about them, Crary said. Still, the hospital does not always succeed. From 2016 to 2018, 10 John and Jane Does remained unidentified during their stays at L.A. County+USC. Some died at the hospital; others
Short-Staffed Nursing Homes See Drop In Medicare Ratings (KHN)

By Jordan Rau and Elizabeth Lucas, Kaiser Health News The federal government accelerated its crackdown on nursing homes that go days without a registered nurse by downgrading the rankings of a tenth of the nation’s homes on Medicare’s consumer website, new records show. In its update in April to Nursing Home Compare, the Centers for Medicare & Medicaid Services gave its lowest star rating for staffing — one star on its five-star scale — to 1,638 homes. Most were downgraded because their payroll records reported no registered-nurse hours at all for four days or more, while the remainder failed to submit their payroll records or sent data that couldn’t be verified through an audit. “Once you’re past four days [without registered nursing], it’s probably beyond calling in sick,” said David Grabowski, a health policy professor at Harvard Medical School. “It’s probably a systemic problem.” It was a tougher standard than Medicare had previously applied, when it demoted nursing homes with seven or more days without a registered nurse. “Nurse staffing has the greatest impact on the quality of care nursing homes deliver, which is why CMS analyzed the relationship between staffing levels and outcomes,” the agency announced in March. “CMS found that as staffing levels increase, quality increases.” The latest batch of payroll records, released in April, shows that even more nursing homes fell short of Medicare’s requirement that a registered nurse be on-site at least eight hours every day. Over the final three months of 2018, 2,633 of the nation’s 15,563 nursing homes reported that for four or more days, registered nurses worked fewer than eight hours, according to a Kaiser Health News analysis. Those facilities did not meet Medicare’s requirement even after counting nurses whose jobs are primarily administrative. CMS has been alarmed at the frequency of understaffing of registered nurses — the most highly trained category of nurses in a home — since the government last year began requiring homes to submit payroll records to verify staffing levels. Before that, Nursing Home Compare relied on two-week snapshots nursing homes reported to health inspectors when they visited — a method officials worried was too easy to manipulate. The records show staffing on weekends is often particularly anemic. CMS’ demotion of ratings on staffing is not as severe as it might seem, however. More than half of those homes were given a higher rating than one star for their overall assessment after CMS weighed inspection results and the facilities’ own measurement of residents’ health improvements. That overall rating is the one that garners the most attention on Nursing Home Compare and that some hospitals use when recommending where discharged patients might go. Of the 1,638 demoted nursing homes, 277 were rated as average in overall quality (three stars), 175 received four stars, and 48 received the top rating of five stars. Still, CMS’ overall changes to how the government assigns stars drew protests from nursing home groups. The American Health Care Association, a trade group for nursing homes, calculated that 36% of homes saw a drop in their ratings while 15% received improved ratings. “By moving the scoring ‘goal posts’ for two components of the Five-Star system,” the association wrote, “CMS will cause more than 30 percent of nursing centers nationwide to lose one or more stars overnight — even though nothing changed in staffing levels and in quality of care, which is still being practiced and delivered every day.” The association said in an email that the payroll records might exaggerate the absence of staff through unintentional omissions that homes make when submitting the data or because of problems on the government’s end. The association said it had raised concerns that salaried nurses face obstacles in recording time they worked above 40 hours a week. Also, the association added, homes must deduct a half-hour for every eight-hour shift for a meal break, even if the nurse worked through it. “Some of our member nursing homes have told us that their data is not showing up correctly on Nursing Home Compare, making it appear that they do not have the nurses and other staff that they in fact do have on duty,” LeadingAge, an association of nonprofit medical providers including nursing homes, said last year. Kaiser Health News has updated its interactive nursing home staffing tool with the latest data. You can use the tool to see the rating Medicare assigns to each facility for its registered nurse staffing and overall staffing levels. The tool also shows KHN-calculated ratios of patients to direct-care nurses and aides on the best- and worst-staffed days. This story originally appeared on Kaiser Health News. Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
