New Jersey Compact Nurse License Bill Passes Senate

A New Jersey compact nurse license bill is one step closer to becoming law after state Senate members passed it last Thursday. The bill passed unanimously, 35-0, with five senators abstaining. The bill would allow New Jersey to join the Nursing Licensure Compact. If approved, New Jersey would be the 32nd state to join the new enhanced NLC which was fully implemented in January 2018. Currently, seven other states also have pending legislation to join the NLC. It would also provide access for New Jersey nurses to practice in its neighbor state Deleware, as well as several other compact states in the Northeast region including Maryland, New Hampshire, Maine, Virginia and West Virginia. Some business associations and nursing groups have thrown their support behind compact nurse license bill in recent weeks, including the New Jersey Business and Industry Association. “I want to first thank Senator Singleton for recognizing the nursing shortage in New Jersey and for introducing legislation that would simplify the process for out-of-state nurses to work in New Jersey,” NJBIA vice president Tony Bawidamann said in a press release. “As a result of his great work, nurses will only need to obtain a license from the state they reside in to be permitted to work in New Jersey, instead of having to go through the whole licensing process again.” One of the largest nursing and healthcare labor unions in the state, Health Professionals and Allied Employees (HPAE), has not endorsed the bill, citing concerns that it could lower the bar for workforce qualifications, according to a report by NJ Spotlight. This is the third time an NLC bill has been introduced since 2015, but the first time that it has made it out of committee and passed through a Senate vote. Senators Troy Singleton, Joseph Vitale and Fred Madden, Jr., sponsored the most recent bill. A companion bill in the New Jersey General Assembly is currently in committee and awaiting a final vote in the Assembly before moving to Gov. Phil Murphy’s desk. The next full Assembly session is scheduled for March 25, according to the state legislature’s website.
Hey, Hey! Ho, Ho! Is Striking For School Nurses The Way To Go?

By Ana B. Ibarra, Kaiser Health News As teachers across the country walk out of their classrooms, hit the picket lines and demand higher pay, they’re keeping school nurses in mind — asking for more of them or, at the very least, better pay for them. Oakland, Calif., teachers plan to strike Thursday if they can’t hammer out a deal with the district that includes a “living wage” and more nurses and counselors. Last week in Denver, thousands of educators and school nurses went on strike and marched to the state Capitol asking for a significant raise — and got it. These unions follow in the footsteps of Los Angeles teachers, who, after striking for six days last month, won a 6 percent salary increase and 300 more school nurses over the next three years, enough to staff every school with a full-time nurse. “It shows that teachers recognize the importance of having a nurse on-site at all times, but it’s sad that it takes a strike to get more nurses,” said Nina Fekaris, president of the National Association of School Nurses and a school nurse in Oregon. Student health is key to academic success, but when it comes to putting nurses in schools, the education system has often “turned a blind eye,” Fekaris said. Now, teachers are making nurses a critical piece of their contract negotiations in a bold move that seems to be working, she said. For districts, it comes down to limited funding, said Erika Hoffman, a lobbyist with the California School Boards Association. “You’ve got massive competing interests: Do I hire a new teacher, a counselor or a school nurse?” School districts do not make these decisions lightly, Hoffman added. “We know healthy kids learn better,” she said. “It’s great that the unions are looking at the needs of the whole child, but [nurses] don’t come for free.” School nurses make a national average salary of $63,944 to $66,973, according to the latest figures from the National Association of School Nurses. About 55 percent of them earn less than $51,000 a year. In many school districts across the country, there simply aren’t enough nurses to tend to students’ medical needs. Nurses often split their time among several campuses, leaving many schools without a nurse at critical times and short of the recommended staffing ratio. In some instances, teachers or support staff administer medication when a nurse isn’t around. And in at least one extreme case, when a gun accidentally discharged inside a Los Angeles Unified School District middle school classroom last year, teachers scrambled to figure out how to tend to the injuries before first responders arrived. Nonetheless, when districts face budget cuts, nurses are among the first staff to go, Fekaris said. That’s because school nurses are not required by law in most states, even though their services, such as vision, hearing and scoliosis screenings, are. The American Academy of Pediatrics used to recommend a ratio of 1 nurse for every 750 students, but the organization updated its recommendation in 2016 to at least one nurse in every school. During the 2017-18 school year, California schools employed 2,623 full-time registered nurses, according to the state Department of Education. With about 6.22 million students enrolled, that averages out to about 1 nurse for every 2,370 students. In West Virginia, teachers went on strike last year and won a 5 percent raise for all staff, including nurses. Now, proposed state legislation would improve the school nurse ratio, which currently stands at 1 nurse to 1,500 students, according to the West Virginia Association of School Nurses. In Los Angeles, the district is still working out how it will pay for the additional 300 nurses it agreed to hire. The union says there’s enough money in the district’s reserve to cover at least the first year of pay for the additional nurses and other support staff. “Our parents really wanted more nurses, and it became one of our top demands,” said Arlene Inouye, secretary of United Teachers Los Angeles. After the strike, Inouye visited Oakland to advise that city’s teachers union, which announced Sunday that it will strike this week, barring “dramatic changes” from the district. “L.A. has been an inspiration,” said Chaz Garcia, a vice president of the Oakland Education Association. “There has been a lot of focus on salaries, but that’s not the driving force and that’s not all we’re looking for,” she said. The union is asking for 1 school nurse for every 750 students “because we do not have enough to deal with students’ growing health issues,” she said. School nurses and teachers in the district are seeing more students with chronic conditions such as asthma, diabetes and food allergies — which require constant monitoring and the administration of medications such as insulin. It’s not that the district doesn’t want to hire nurses, said Andrea Bustamante, executive director of student services at Oakland Unified School District. It’s that it can’t. The district, which has about 37,000 students, budgets for 32 nurses, but seven of those positions are vacant, she said. “Like many other California districts, we have struggled to find qualified candidates to fill our vacancies,” Bustamante said in a written statement. She cited obstacles including the additional state certification required to become a school nurse and competition from hospitals. What school districts really need to do if they want to attract more nurses is offer them a “living wage,” said Sean McFarland, a school nurse at Denver Public Schools who participated in the strike there. Before working in schools, McFarland was a charge nurse in an emergency room, where he made about $16,000 more a year than his starting salary at the school district, he said. He took the pay cut because he wanted to try nursing in another setting and give back to his community in a different way, he said. When he started, he befriended four other new nurses. “Out of the five of us, I am the only one who
US Measles Cases Surpass 2016, 2017 Totals, CDC Reports
The number of measles cases in 2019 has already surpassed annual totals for 2016 and 2017, according to a recent Center for Disease Control and Prevention report. At least 127 cases have been recorded this year as of last Thursday, which is an increase of 48 more cases since February 4. The annual totals for 2016 and 2017 were 86 and 120, respectively. CDC officials linked the spread of measles cases to unvaccinated travelers who have brought the virus back from countries experiencing large measles outbreaks, like Ukraine and Israel. Individual measles cases have occurred in California, Colorado, Connecticut, Georgia, Illinois, Kentucky, New York, Oregon, Texas and Washington. Five outbreaks, defined as three or more cases recorded in an area, have occurred in New York, Texas and Washington. Among all of the recorded cases, Washington has been hit the hardest by the spread of measles. Almost half of all measles cases—64 in total as of Thursday—have occurred in Washington state’s Clark County, according to a recent report by Center for Infectious Disease Research and Policy (CIDRAP). Washington Gov. Jay Inslee declared a state of emergency in late January, directing state agencies and departments to divert as many resources as possible to assist affected areas. While 2019 has seen a sharp increase in measles cases, 2014 holds the record of the most cases in the past decade, according to CDC data. A total of 667 cases were recorded in 2014, more than half of which occurred in one outbreak among an unvaccinated Amish community in Ohio.
5 Reasons Why Travel Nurses Would Actually Want To Work Night Shift

By Alex McCoy, Contributing Writer, Owner of Fit Travel Life My relationship with the night shift has always been a tenuous balance between love and hate. Being on day shift allows for a more normal routine and definitely makes my husband more at peace with my work schedule. The feeling of being fully rested on my off days has led me to continue taking day shift assignments, but there is always a small piece of me that is envious when I meet the new night shift crew. Night shift has plenty of downsides–less support staff on duty, irregular sleep schedules, and more difficulty contacting physicians are just a few of the problems any night shift nurse could list for you. But at the end of the day, there is a reason many travel nurses prefer nights even if travel contracts don’t come with a hefty night shift differential. Less support staff at night means night shift travel nurses don’t have to learn extra procedures for working with these staff members. via GIPHY One of the first things I ask about at each new assignment is how to contact people I have to coordinate care with on day shift. Whether you are trying to contact a social worker or order lunch, there is a different procedure for these tasks at each hospital. If you work the night shift, you have the blessing—and the curse—of not having access to most of these extra pieces. While missing out on the support may cause some stress, it is nice to know you don’t have to relearn these procedures because they simply don’t apply to your shift. Unless it is a rare exception, the night shift gets to skip over this piece of knowledge when zipping through each new orientation. Less pressure from management or less involvement in unit politics. via GIPHY I wrote a whole article on the reasons why travel nurses should avoid hospital politics. The bottom line is: it’s much harder to accomplish this during the day shift. One of my least favorite scenarios is having a manager wander through on day shift and stop to ask my opinion on the unit. I appreciate the fact that they are looking for constructive feedback, but I also like to have more time to think through responses and articulate my feelings. As a night shifter, you are much less likely to get pulled into these types of conversations. If a manager is looking for some feedback it will be easier to strike up that conversation via email. For me, I prefer this method because I can still give meaningful feedback without becoming too involved in whatever issues the manager is trying to address. Patients are less likely to need to be prepped for procedures and testing. via GIPHY Another policy that can change drastically between assignments is pre- and post-procedure policy. I have seen several variances from how a patient is transported to how frequently nurses monitor post-op vital signs. I very rarely had to know the details of these procedures on the night shift. Except for rare emergent cases, my patients rarely left the floor at night. I was especially thankful as a new traveler to not have to learn the ins-and-outs of consents and transport when I was desperately trying to pick up on all the other new procedures during my short orientation. The night shift lull can be a great time to get to know your coworkers. via GIPHY During the day shift, the 2-4 p.m. period can be one of the busiest. This is when baths are fit in, discharges and admissions become a revolving door, and all the catch-up charting happens before starting the 4 p.m. rounds. On the night shift, this is what I liked to refer to as the “golden period.” Once your midnight rounds are done you inevitably cross your fingers and hope for no excitement during this chunk of the night. Some of my favorite memories as a night shift nurse were made during this time frame, where patients are finally sleeping for a bit and families have calmed down enough to get a bit of rest themselves. As a traveler, this is when you have time to get to know your coworkers. Use this to your advantage and strike up conversations or share some stories to make the shift go a little faster for everyone. Breakfast drinks are a great icebreaker to meet new friends. via GIPHY There is a weird bond that can only be formed over a glass of local beer at 8 a.m. in the dingy bar two blocks from the hospital. If you are feeling shy or struggling to make friends at your new assignment, one of my favorite ways to break the tension is to ask about the favorite night shift hangout. I have found that once you have a breakfast and beer date with new coworkers, a wall comes down that allows for more camaraderie and connection at work. Even though I enjoy having a normal schedule and not having to nap on my days off, as a traveler I truly do miss working the night shift. There is a certain bond that all night shifters share and I don’t feel like day shift has quite the same connection. I absolutely loved my night shift assignments and felt they were less stressful for reasons other than the stereotypical “Oh, it must be easy because all of your patients are sleeping” (Hard eye roll to that statement). Even if the money doesn’t necessarily change between day and night shift for travelers, I certainly understand the draw many nurses would feel to work nights as a travel nurse and am thankful for those who love the nocturnal life and adjust to it so well. Alex McCoy currently works as a pediatric travel nurse. She has a passion for health and fitness, which led her to start Fit Travel Life in 2016. She travels with her husband, their cat, Autumn and
Hawaii, Indiana, Washington Introduce Nursing Licensure Compact Legislation In 2019

Exactly a year and one month ago, the National Council of State Boards of Nursing (NCSBN) enacted the enhanced Nursing Licensure Compact—referred to as the NLC—with the goal of streamlining the compact license requirements and adding an extra layer of security by requiring federal background checks for all applicants. A total of 31 states have joined the NLC since January 19, 2018, including Kansas and Louisiana, which both passed legislation to join last year and are expected to fully implement their NLC programs by July 1. They weren’t the only states interested in joining the NLC last year. Illinois, Michigan, New York, Vermont, Massachusetts, Rhode Island and New Jersey all had pending legislation last year to join the NLC. Of those states, only New Jersey, Massachusetts, Indiana and Michigan still have legislation pending. Three new states—Hawaii, Indiana and Washington—have all introduced some form of legislation related to the NLC earlier this year that could result in three new compact states. While it’s unlikely that these states will implement NLC programs this year, we’ve provided a breakdown of the issues surrounding each piece of legislation, and if they will realistically pass muster with their state governments. Breakdown of potential new nursing compact license states Hawaii What legislation is in the works? Hawaii does not have a bill to actually join the NLC, but on January 24, House Rep. Ichiyama Takumi introduced a bill that would establish a study to identify potential issues that could arise if the state joins the NLC. How much progress has it made so far? As of February 16, the bill has been recommended for approval almost unanimously by every House committee assigned to review it, including the Consumer Protection and Commerce, Health and Intrastate Commerce committees. The bill is scheduled for a final review with the Finance committee on February 21. Why is this a big deal? While it’s not technically legislation to join the NLC, it’s still big news that Hawaii lawmakers are considering joining in the first place. If the results of the study are favorable and NLC legislation is introduced, Hawaii could become the first non-continental state to join the compact. Hawaii is already an incredibly popular destination state for travel nurses, but it could be even more popular if its made accessible for compact license holders. It could incentivize native Hawaii nurses to travel as well since they would gain more than 30 additional states to practice in if NLC legislation is approved. What are the chances it will actually pass? Very high. Almost every committee assigned to review it has recommended it for approval and are moving it quickly through the House, so there is a solid chance the bill could pass through the House by the end of February. Indiana What legislation is in the works? House Bill 1344, introduced on January 14 by Republican Rep. Edward Clere, would allow for Indiana to join the Nursing Licensure Compact. How much progress has it made so far? The NLC legislation passed unanimously in the Indiana House on January 31 and is making its way through various committees in the state Senate as Senate Bill 436. Why is this a big deal? If Indiana passes legislation to join the NLC, not only would compact license travelers have access to a new state, but it would allow for Indiana nurses to practice across the Indiana-Kentucky state line in Louisville—an issue that is frequently brought up by compact license advocates when addressing gaps in nursing service. It would also allow for nurses without a single-state license but who have a compact license to possibly start jobs quicker, as it can currently take several weeks to obtain a permanent nursing license in Indiana. What are the chances it will actually pass? Very high. This is the second time Rep. Ed Clere has introduced NLC legislation after his first attempt in 2018 with House Bill 1317, which urged legislators to conduct a study into the impact of joining the compact, among several other provisions. The bill went into a legislative study over last summer to address any concerns, and since then has gained significant momentum and support among lawmakers, according to a Komoko Tribune report. The current NLC bill also has the support of several healthcare associations and interest groups, including Baptist Health Floyd, One Southern Indiana, the Indiana Hospital Association and the Coalition of Advanced Practice Nurses of Indiana, according to the Indiana Chamber. Washington What legislation is in the works? Washington House Bill 1882 and Senate Bill 5460 were both introduced this year and would allow Washington to join the NLC. How much progress has it made so far? Both bills have moved to committee for further discussion and debate. The Senate Health & Long Term Care Committee public hearing on February 1 can be found here. Why is this a big deal? If implemented, Washington would be the first state on the West coast to join the NLC. It would also allow for Washington nurses to practice across the Washington-Idaho state line, as Idaho is already a part of the NLC. What are the chances it will actually pass? Mixed. Some members of the business and military sector in Washington, as well as the NCSBN, support the state joining the NLC, according to several testimonies given on February 1 during a Senate Health and Long Term Care Committee hearing. “We have, as a state, already passed the Physical Therapy Licensure Compact and the [Interstate] Medical Licensure Compact, and we’ve done so because we know the compacts are effective,” Sen. Annette Cleveland, a sponsor for the bill, said during the hearing. “31 other states…already have nurse licensure compacts, others are also considering joining, and I want to ensure our state is also having that conversation.” The Washington State Nurses Association (WSNA) opposes the bill, according to a Senate committee testimony by Melissa Johnson, a spokesperson for the WSNA. Some of the concerns of the WSNA include a lack of need for the compact with the state board’s
Shrinking Medicaid Rolls In Missouri And Tennessee Raise Flag On Vetting Process

By Phil Galewitz, Kaiser Health News Tangunikia Ward, a single mom of two who has been unemployed for the past couple of years, was shocked when her St. Louis family was kicked off Missouri’s Medicaid program without warning last fall. She found out only when taking her son, Mario, 10, to a doctor to be treated for ringworm. When Ward, 29, tried to contact the state to get reinstated, she said it took several weeks just to have her calls returned. Then she waited again for the state to mail her a long form to fill out attesting to her income and family size, showing that she was still eligible for the state-federal health insurance program for the poor. Mario, who is in third grade, missed much of school in December because Ward could not afford a doctor visit without Medicaid. His school would not let him return without a doctor’s note saying he was no longer infected. In January, with the help of lawyers from Legal Services of Eastern Missouri, she was able to get back on Medicaid, take her son to a doctor and return him to school. “It was a real struggle as it seemed like everyone was giving me the runaround,” Ward said. “I am upset because my son was out of school, and that pushed him behind.” Ward and her children are among tens of thousands of Medicaid enrollees who were dropped by Missouri and Tennessee last year as both states stepped up efforts to verify members’ eligibility. Last year, Medicaid enrollment there declined far faster than in other states, and most of those losing coverage are children, according to state data. State health officials say several factors, including the improved economy, are behind last year’s drop of 7 percent in Missouri and 9 percent in Tennessee. But advocates for the poor think the states’ efforts to weed out residents who are improperly enrolled, or the difficulty of re-enrolling, has led to people being forced off the rolls. For example, Tennessee sent packets to enrollees that could be as long as 47 pages to verify their re-enrollment. In Missouri, people faced hours-long waits on the state’s phone lines to get help in enrolling. Medicaid enrollment nationally was down about 1.5 percent from January to October last year, the latest enrollment data available from the federal government’s Centers for Medicare & Medicaid Services (CMS). Herb Kuhn, president and chief executive of the Missouri Hospital Association, said the state’s efforts to verify Medicaid eligibility could be tied to an increase in the number of people without coverage that hospitals are seeing. “When we see over 50,000 children come off the Medicaid rolls, it raises some questions about whether the state is doing its verifications appropriately,” he said. “Those who are truly entitled to the service should get to keep it.” In 2018, Missouri Medicaid began automating its verification system for the state-federal insurance program for the poor. People who were identified as ineligible, for income or other reasons, were sent a letter asking them to provide updated documentation. Those who did not respond or could not prove their eligibility were dropped. The state does not know how many letters it sent or how many people responded, said Rebecca Woelfel, spokeswoman for the Missouri Department of Social Services, which oversees Medicaid. She said Missouri Medicaid enrollees were given 10 days to respond. Woelfel cited the new Medicaid eligibility system, the improved economy and Congress rescinding the federal tax penalty for people who lack insurance as factors behind the decline in enrollment. Missouri’s unemployment rate dropped from 3.7 percent in January 2018 to 3.1 percent in December as the number of unemployed people fell by about 17,000. Missouri Medicaid had almost 906,000 people enrolled as of December, down from more than 977,000 in January 2018, according to state data. About two-thirds of those enrolled are children or pregnant women. Timothy McBride, a health economist at Washington University in St. Louis who heads a Missouri Medicaid advisory board, said the state’s Medicaid eligibility system has made it too difficult for people to stay enrolled. Since low-income people move or may be homeless, their mailing addresses may be inaccurate. Plus, many don’t read their mail or may not understand what was required to stay enrolled, he added. “I worry some people are still eligible but just did not respond, and the next time they need health care they will show up with their Medicaid card and find out they are not covered,” McBride said. Tennessee’s Medicaid enrollment fell from 1.48 million in January 2018 to 1.35 million in December, according to state data. Tennessee Medicaid spokeswoman Kelly Gunderson credits a healthy job market. The state’s unemployment rate was relatively stable last year at under 4 percent. “Tennessee is experiencing a state economy that continues to increase at what appears to be near-historic rates, which is positively impacting Tennesseans’ lives and, in some cases, decreasing their need to access health insurance through the state’s Medicaid” program and the Children’s Health Insurance Program (CHIP), she said. She added that the state has a “robust appeals process” for anyone who was found ineligible by the state’s reverification system. The Tennessee Justice Center, an advocacy group, has worked with hundreds of families in the past year trying to restore their Medicaid coverage. The verification process will make “Medicaid rolls smaller and saves money, and that’s a poor way for the state to measure success,” said Michele Johnson, executive director of the nonprofit group. “But it’s penny-wise and pound-foolish” because it leads to people showing up at emergency rooms without coverage — and hospitals have to pass on those costs to everyone else. After rapid growth since 2014, when the Affordable Care Act expanded health insurance coverage to millions of Americans, Medicaid enrollment nationally started to fall, declining from 74 million in January 2018 to about 73 million in October, according to the latest enrollment data released by CMS. Missouri and Tennessee are among 17
Tall Man, Tall Van: Nate Hemann Shares His Experience Travel Nursing While Living The Van Life

Like many travel healthcare professionals, nurse Nate Hemann wanted to pursue traveling to experience new sights, meet new people and gain experience working across the country. Before starting his journey, Hemann decided to make his first major commitment to the travel life in an unconventional way—by converting a freshly purchased 2018 Ford Transit into his permanent home away from home. Hemann started documenting his experience building and living in his van on August 2, 2018, through his Instagram account, @thetallmanvan. From his posts, Hemann shares messages of positivity, his enthusiasm for nature and all the highs and lows of living in a van while working as a travel nurse. I spoke with Hemann to find out more about his nursing career, how he converted his ride and why he decided to tackle the #VanLife. Editor’s Note: Photos in this story pulled from the @thetallmanvan account were used with permission. Some of the answers below were edited for clarity. Q: How did you get involved in the nursing profession? I decided I was going to go to school for nursing in about the 10th grade. I honestly don’t remember a single moment that sparked it. I did, however, grow up right next to the Mayo Clinic, and with both of my parents working there, as well as nearly every other adult in my life growing up, it’s really no surprise that I ended up with a career in the medical field. I have also always loved people and science, and to me, nursing is the best fit for me with my strengths in both of those areas. Q: What made you want to pursue the travel nursing route? Travel nursing was not something I had ever thought about until holiday break during my senior year of nursing school. I went on a study abroad trip with 20 some other nursing students to the Philippines to learn about and dive into the culture and nursing practices there. This single trip set me on the travel path that I am on now, both in my career and in my personal life. I made it a financial goal of mine after graduating college to always be able to say “yes” to travel when asked by anyone around me, and so far, I’m surpassing my goal of traveling whenever possible far more than I ever imagined I would. Q: Being that you’ve just started your travel career, what has the experience been like so far? Although I technically began my travel nurse career the beginning of October 2018, I feel that it really started in July of 2017. After working one year as a staff nurse in Duluth, Minnesota, I packed up my car and drove to Seattle to be a part of the amazing team and culture of Harborview Medical Center. After a year at Harborview, and meeting all of the countless, amazing travel nurses there, I knew that I had to be one as well. View this post on Instagram A post shared by Nate Hemann (@thetallmanvan) on Feb 6, 2019 at 6:59am PST The experience so far has been supportive and educational, as well as beautiful considering I have gotten to be in Northern California and Central Oregon for my first two contracts. I feel fortunate to have gone to two hospitals so far with an overall good attitude toward travel nurses because I know that that is not always the case. Q: What have you learned? Any unexpected challenges? I have learned that I love to float, which as a traveler is something you have to learn to like, or you certainly won’t have a good experience. I love the challenge of a new unit and a new patient demographic outside of my specialty. I will say that I am not learning as much nursing-wise as I would like to, and that’s why I will seek out more trauma and teaching hospitals, like Harborview. For now, I am trying to keep up to date outside of work. However, I am learning so much about myself being in these smaller cities and hospitals. It is giving me more financial freedom and time to explore the great outdoors with my van and any friends I meet along the way. As far as nursing goes, the main challenge I have found is that staff nurses tend to be resistant to change, and as the new nurse on the unit all the time, that can make me feel isolated. I have picked up skills and knowledge in various ways and places, and some nurses I work with only know nursing from the college in the same community that they work in—and perhaps have lived in that very community their entire life. As someone who constantly wants to learn and understand the world from other perspectives, it frustrates me to work with complacent and inflexible individuals. Q: Where have you visited so far? Considering that, what’s your most favorite moment from the places you have visited? My two contracts so far have been in Eureka, California and Eugene, Oregon. I have visited countless places outside of these two locations since I drove from Minnesota to get here, and in between contracts, I took two-and-a-half weeks off to ski in Wyoming and Utah. Top of my list since starting travel nursing would be as follows in no particular order: Grand Teton National Park, Lassen Volcanic National Park, Redwoods National Park, and the Southern Oregon coast. View this post on Instagram A post shared by Nate Hemann (@thetallmanvan) on Oct 19, 2018 at 11:24am PDT I’m not typically a man of favorites—usually a top three or five kind of guy—but there was an instance during this travel nurse journey that I felt absolute bliss. I hiked down a steep and wooded part of the Southern Oregon coast, made my way to rocky outcrops, and it was all just after a big storm system had rolled through. The waves crashing against the coast were absolutely massive. I
Travel Jobs: ‘Hot’ February 2019 Market Means More Location Variety, Fewer Premium Pay Options

As the last month of the busy winter season marches on, one of the main concerns circling around the travel healthcare community in recent weeks is the high amount of low-paying contracts advertised by recruiters or posted by agencies. While there is a kernel of truth in those concerns, recruiters and agency sales representatives say that the answer is not so simple. The travel nurse market is hot on both sides of the fence—healthcare facilities across the country have plenty of urgent needs, and lots of potential candidates are available and looking for work, said Oren Lavi, a director of client advisory for LiquidAgents Healthcare. “The market is hotter than it has been in the last 24 months. The time to jump in is now,” said Oren Lavi, a director of client advisory for LiquidAgents Healthcare. “More jobs means more variety. Hospitals are not going to list premium pay packages unless they see the nurse pool drying up. For now, the candidate pool is consistent so they have no reason to raise rates.” Some exceptions to this trend include northeastern states like Pennslyvania and New Hampshire, and Midwest states like Wisconsin, Illinois and Michigan. Similar to our January predictions, cold weather is keeping seasonal travelers away, which mean travelers are more likely to find premium pay packages—$1,800 and up per week before taxes—in these areas. Additionally, most of the northern and Midwest states where bill rates have remained consistently high over the winter also saw a spike in traveler job applications in January, according to StaffDNA job board data. Travel Healthcare Job Market for February 2019 Here’s a quick breakdown of the states and travel healthcare job specialties that are most-in-demand now and are expected to stay popular in February, according to data provided by industry sales and recruiting representatives. Arkansas RN: Medical-surgical, telemetry, step-down/PCU Illinois RN: Medical-surgical, telemetry, ER, labor and delivery Indiana RN: Medical-surgical, telemetry. Much higher needs compared to January, close to 100 open positions as of February 8. Job submittals around Indianapolis close within 24 hours. Kentucky RN: Medical-surgical, telemetry, step-down/PCU Missouri RN: Medical-surgical, telemetry, ER (On the lower end, but needs are increasing). All core specialties in demand in St. Louis. Allied: X-ray/radiology techs New Hampshire RN: Medical-surgical, telemetry. Bill rates much higher than average. Surgical Tech: OR Oklahoma RN: Medical-surgical, telemetry. Job needs are filling very quickly. Pennsylvania RN: ICU, OR, medical-surgical, telemetry Texas RN: Medical-surgical, telemetry, step-down/PCU January 2019 Top Markets Editor’s note: This list is created by analyzing the number of travelers applying for jobs in these individual states and Washington D.C. This data is not necessarily a historical indicator of job volume. Application data comes from the StaffDNA jobs database. Florida Texas California South Carolina Georgia Pennsylvania Tennessee Arizona Michigan North Carolina Indiana Arkansas Kentucky Missouri New Mexico Oklahoma Virginia West Virginia Iowa Nevada Oregon Wisconsin Idaho Maine Colorado Alaska Hawaii Illinois Ohio Washington Alabama Louisiana Massachusetts Connecticut Kansas Mississippi Maryland Minnesota New Hampshire New Jersey Utah Vermont Wyoming Washington D.C. Deleware Montana North Dakota Nebraska New York Rhode Island South Dakota
Baylor Scott & White, Memorial Hermann Health Mega Merger Called Off

Two major Texas hospital systems, Baylor Scott & White Health in Dallas and Memorial Hermann Health System in Houston, called off a mega merger deal Tuesday that would have created the largest hospital system in the state. No specific reason was given for the cancellation. “After months of thoughtful exploration, we have decided to discontinue talks of a merger between our two systems. Ultimately, we have concluded that as strong, successful organizations, we are capable of achieving our visions for the future without merging at this time,” a hospital spokesperson said in a joint statement. “We have a tremendous amount of respect for each other and remain committed to strengthening our communities, advancing the health of Texans and transforming the delivery of care. We will continue to seek opportunities for collaboration as two forward-thinking, mission-driven organizations.” If the merger had passed, the system would have managed 68 hospitals and more than 73,000 employees. It also would have created one of the largest not-for-profit systems by revenue, according to Modern Healthcare. Baylor Scott & White Health and Memorial Hermann Health signed a letter of intent in October to merge “to further strengthen communities, advance the health of Texans and transform the delivery of healthcare.” Another huge year for hospital, healthcare mergers While this mega merger deal fell through, several other major joint ventures made headlines in 2018, capping off another year of increased mergers and acquisitions activity in the healthcare industry. The total volume of deals increased by 14.4 percent from 2017 to 2018, according to an analysis by PricewaterhouseCoopers, although the value of those deals declined more than 30 percent, and slowed some in Q4. Of all the healthcare deals in 2018, the largest and most notable was CVS Health’s acquisition of Aetna for $69 billion, which was finalized in November. “Today marks the start of a new day in healthcare and a transformative moment for our company and our industry,” CVS Health President and Chief Executive Officer Larry J. Merlo said in a press release. “By delivering the combined capabilities of our two leading organizations, we will transform the consumer health experience and build healthier communities through a new innovative health care model that is local, easier to use, less expensive and puts consumers at the center of their care.” Healthcare leaders are still waiting to see how this landmark deal will impact the industry and marketplace, and providers are wary that the merger could create a landscape that incentivizes use of urgent care centers and retail clinics over traditional healthcare facilities, according to a report from Revcycle Intelligence. Merger and acquisition activity in 2019 is expected to remain strong, although healthcare executives expect the actual volume of activity will level out, according to a recent survey by Capital One.
Transparent Hospital Pricing Exposes Wild Fluctuation, Even Within Miles (KHN)
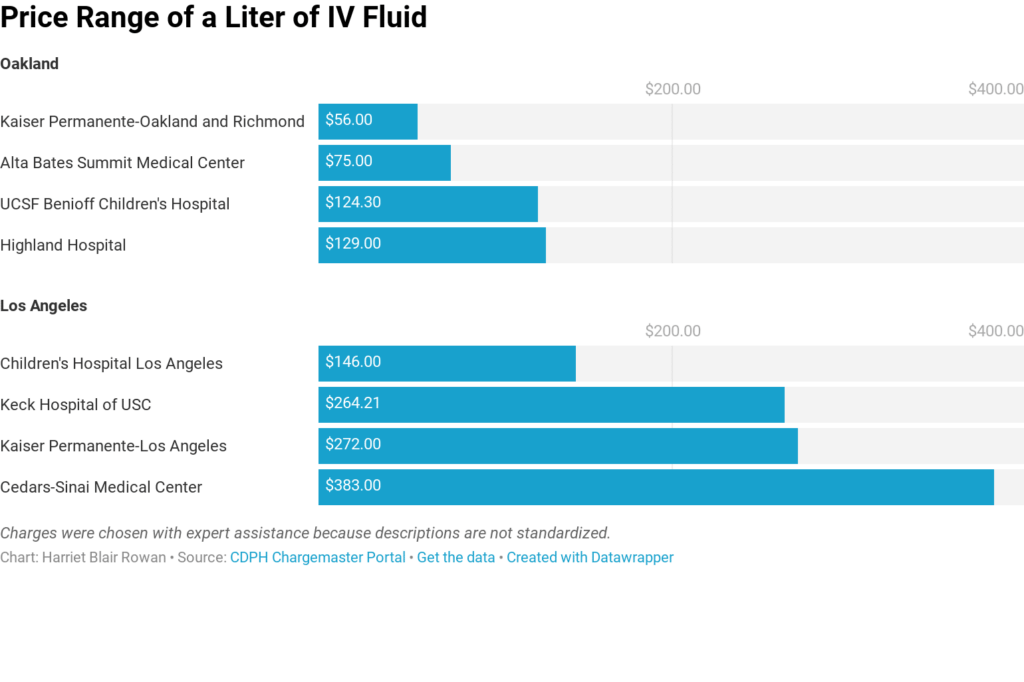
By Harriet Blair Rowan, Kaiser Health News The federal government’s new rule requiring hospitals to post prices for their services is intended to allow patients to shop around and compare prices, a step toward price transparency that has generated praise and skepticism. Kaiser Health News examined the price lists — known in hospital lingo as “chargemasters” — of the largest acute care hospitals in several large cities. Prices varied widely on some basic procedures, even for basic charges. For instance, the list price on a liter of basic saline solution for intravenous use ranged from $56 to $472.50, nearly seven times as much. A brain MRI with contrast was priced from $1,7210 to $8,800 at the hospitals. And they varied widely even when comparing nearby hospitals. The new rule mandates that the chargemasters be available on the hospital website in a machine-readable format, but not all hospitals make them easy to find, and understanding them is a bigger obstacle. (Story continues below.) KHN senior correspondent Julie Appleby and California Healthline’s Barbara Feder Ostrov recently wrote about this new rule and found price lists befuddling to most anyone without an advanced medical degree. This story first appeared on California Healthline, and later on Kaiser Health News. Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
