New ‘Healthcare Travelers Take Omaha’ Conference Set For Early April

Travel healthcare professionals have said pursuing a travel career can be a lonely experience. Travelers are spread all across the country, which can make it difficult to connect with their colleagues outside of social media. So when the idea for a new travel healthcare conference came about during TravCon 2018, it wasn’t out of a desire to create a competing conference, but instead to provide another event where travelers can network and connect, travel nurse Thomas Piper said. “We wanted to provide people another option to supplement TravCon,” Piper said. “Not everyone can make it to Vegas every year in September, so this conference is another place where travelers can connect.” Piper is helping organize the new conference Healthcare Travelers Take Omaha, which is set to take place from 8 a.m. to 5 p.m. on April 5-6 at the Holiday Inn Omaha Downtown-Airport in Omaha, Nebraska. Tickets cost $50, which covers the cost of food provided during the conference, Piper said. Only 150 tickets will be sold and the number of travel company exhibitors for the event is capped at 30, Piper said. So far, around 20 percent of the tickets have been sold, but Piper said he expects that number to increase as travelers settle into their first contracts of the year and plan time off. As of Wednesday, 21 of the 30 exhibitor slots have been filled, according to the conference website. Piper’s traveler Facebook group Scrub Squad 1978 along with Gypsy Soul Travel Nurses and Adventures In RV Travel Nursing are the official hosts for the event, according to their website. Along with a keynote speaker, recruiter panel and CEO panel discussion, the conference plans to offer several learning sessions with industry professionals and special group events, including a charity golf tournament benefiting autism research, a 5K fun run/walk and a meet-and-greet mixer. The learning sessions will cover topics like traveler taxes, fitness on the road, breaking a contract, RV travel and housing, according to their website. Small setting, good conversation Part of the reason why Healthcare Travelers Take Omaha is only accepting a small number of travelers and exhibitors is out of necessity, Piper said. Planning for the conference began in April, so with only six months to pull the event together, venue options were fairly limited. Organizers also wanted to keep the cost of entry as low as possible for both attendees and exhibitors, which is why Omaha was selected for the first year of the conference, Piper said. “Omaha is a central hub for travel nursing companies,” Piper said. “It’s also centrally located, so it’s very inexpensive for travelers to access who may be on the edges of the country.” More than a dozen travel healthcare staffing companies call Omaha home, including Aureus Medical Group, Atlas Medstaff and Fusion Medical Staffing, all of which are exhibitors for the event. The conference won’t be held in Omaha every year, however. Another reason why organizers wanted a different conference was a chance to meet up with travelers in new places, Piper said. Organizers are already looking ahead to next year’s conference in Orlando where they plan to offer more tickets for travelers and space for exhibitors. “We’re travelers—we like to travel the country and don’t want to go to the same city every year,” Piper said. “TravCon is great and a lot of fun. I plan on going to it every year. But it can be expensive to visit Vegas every year if you’re working on the East Coast or want to bring your family along.” Another reason why organizers wanted a smaller setting was to offer more time for travelers and companies to network with each other, Piper said. “We’ve set a lot of time aside for people to have actual conversations with agencies and recruiters,” Piper said. “It’s definitely going to be a more intimate setting for networking and forming relationships.” Piper was encouraged by how quickly Healthcare Travelers Take Omaha has come together and hopes this conference will provide another great option for travelers to connect with each other, he said. “Talking after TravCon last year, we weren’t sure we would be able to throw it all together within six months, but it’s coming along nicely,” Piper said.
Why Travel PTs Should Consider Home Health Jobs In 2019

By Stephen Stockhausen, PT, DPT, OCS, Contributing Writer, Founder of PT Adventures As 2019 rolls in we all have change on our minds. Sometimes it is something as simple as a New Year’s resolution—that chances are you have already broken—or occasionally it is something much bigger, like changing your job. For those of you considering the latter, I am here to tell you that taking a contract in home health might be one short-term change that you stick with all year. Why Travel PTs Should Consider Home Health In 2019 1. Join the Party via GIPHY With patients being discharged “sicker and quicker” from hospitals, and skilled nursing facilities incentivized to do the same come October of this year via the Patient-Driven Payment Model, a considerable uptick in home health admissions is to be expected. Early Release After Surgery (ERAS) total joint patients are popping up with increasing frequency on home health case loads. With clients foregoing the 2-5 days in a hospital bed, they are able to get up and moving much quicker under the care of a home health physical therapist. This is a growing field by all accounts. The travel physical therapist who has experience in this high demand field will find themselves sought after for jobs in locations where they previously could not find work. Building a stronger resume in more settings will only serve to boost your chances of landing a job in that dream location or at your goal pay rate. 2. Mo’ Money, Fewer Problems via GIPHY Speaking of pay rates, did I mention that home health is one of, if not the most, high paying setting in physical therapy? It is not unheard of for travel home health physical therapists to make over $2,200 per week after taxes. Add a 40 hour guaranteed contract on top of that and you have a sweet paying gig regardless of patient census. My wife and I were able to pay off around $240,000 in combined student loan debt in three years using home health jobs almost exclusively! You can read more about that story here. 3. Freedom via GIPHY Despite all of the exciting, challenging, and lucrative aspects of home health, it may be the freedom that is the most impactful for clinicians new to the setting. For most agencies, a full day in home health is 4-6 patients, and depending on visit type, sometimes only two patients are required. Making things even better, at nearly all companies you get to make your own schedule. Mani-pedis with the girls after a long lunch? Want to squeeze in a mid morning trail run? Perfect! Just call your clients and move your day around accordingly. My wife and I have our 18-month-old daughter with us on the road, and because we are both working home health jobs we can arrange it so that we only have a nanny at our home for around five hours a day. That’s hard to accomplish in most other travel job settings. Now, I do not want to mislead you. You will likely end up putting in your 40 hours for the week. The documentation and driving can eat into your working time more than you’d expect, but at least you are getting paid for mileage. Still, with most systems you can document from anywhere you can get Internet service. Nestled deep into your couch, on top of a bluff overlooking the beach, or even from the patio of a beautiful vineyard. The choices are endless, and they are all available to you. Years ago, back in PT school, it was made abundantly clear to us that home health is where therapists go to disappear. Substandard care was not the exception, but the rule, and none of us students should stoop to level occupied by the lowly home health PT. Well, I’m here to tell you that this could not be further from the truth. Things have changed in the three years between PT school and taking my first home health job. There is an abundance of superior clinicians making their way into the home health setting. OCS, GCS, and NCS clinicians, traditionally found in outpatient or acute/subacute care are migrating to home health with increasing frequency. Maybe it is the challenge, the excitement of a growing field, the money or the freedom. Whatever it is, clinicians are making a change in their lives and giving home health a try. Maybe this year is the right time for you to do the same. Stephen Stockhausen is a doctor of physical therapy, a traveler, and a founder of PT Adventures—a blog created with his wife Ellen to help travel PTs take control of their career and live their dreams. You can find Stephen and Ellen exploring the country with their daughter, Kinley, and two dogs Cayenne and Layla.
Analysis: Can States Fix The Disaster Of American Healthcare? (KHN)
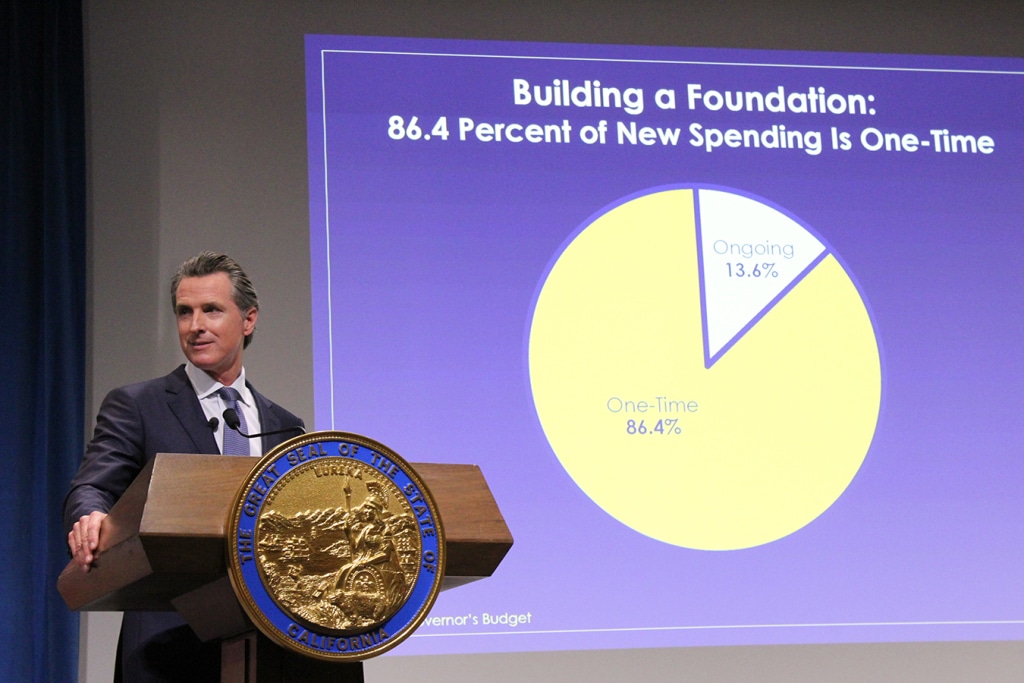
By Elisabeth Rosenthal, Kaiser Health News Last week, California’s new governor, Gavin Newsom, promised to pursue a smörgåsbord of changes to his state’s healthcare system: state negotiation of drug prices, a requirement that every Californian have health insurance, more assistance to help middle-class Californians afford it and healthcare for undocumented immigrants up to age 26. The proposals fell short of the sweeping government-run single-payer plan Newsom had supported during his campaign — a system in which the state government would pay all the bills and effectively control the rates paid for services. (Many California politicians before him had flirted with such an idea, before backing off when it was estimated that it could cost $400 billion a year.) But in firing off this opening salvo, Newsom has challenged the notion that states can’t meaningfully tackle healthcare on their own. And he’s not alone. A day later, Gov. Jay Inslee of Washington proposed that his state offer a public plan, with rates tied to those of Medicare, to compete with private offerings. New Mexico is considering a plan that would allow any resident to buy in to the state’s Medicaid program. And this month, Mayor Bill de Blasio of New York announced a plan to expand healthcare access to uninsured, low-income residents of the city, including undocumented immigrants. For over a decade, we’ve been waiting for Washington to solve our healthcare woes, with endless political wrangling and mixed results. Around 70 percent of Americans have said that healthcare is “in a state of crisis” or has “major problems.” Now, with Washington in total dysfunction, state and local politicians are taking up the baton. The legalization of gay marriage began in a few states and quickly became national policy. Marijuana legalization seems to be headed in the same direction. Could reforming healthcare follow the same trajectory? States have always cared about healthcare costs, but mostly insofar as they related to Medicaid, since that comes from state budgets. “The interesting new frontier is how states can use state power to change the healthcare system,” said Joshua Sharfstein, a vice dean at Johns Hopkins Bloomberg School of Public Health and a former secretary of the Maryland Department of Health and Mental Hygiene. He added that the new proposals “open the conversation about using the power of the state to leverage lower prices in healthcare generally.” Already states have proved to be a good crucible for experimentation. Massachusetts introduced “Romneycare,” a system credited as the model for the Affordable Care Act, in 2006. It now has the lowest uninsured rate in the nation, under 4 percent. Maryland has successfully regulated hospital prices based on an “all payer” system. It remains to be seen how far the West Coast governors can take their proposals. Businesses — pharmaceutical companies, hospitals, doctors’ groups — are likely to fight every step of the way to protect their financial interests. These are powerful constituents, with lobbyists and cash to throw around. The California Hospital Association came out in full support of Newsom’s proposals to expand insurance (after all, this would be good for hospitals’ bottom lines). It offered a slightly less enthusiastic endorsement for the drug negotiation program (which is less certain to help their budgets), calling it a “welcome” development. It’s notable that his proposals didn’t directly take on hospital pricing, even though many of the state’s medical centers are notoriously expensive. Giving the state power to negotiate drug prices for the more than 13 million patients either covered by Medicaid or employed by the state is likely to yield better prices for some. But pharma is an agile adversary and may well respond by charging those with private insurance more. The governor’s plan will eventually allow some employers to join in the negotiating bloc. But how that might happen remains unclear. The proposal by Washington Gov. Inslee to tie payment under the public option plans to Medicare’s rates drew “deep concern” from the Washington State Medical Association, which called those rates “artificially low, arbitrary and subject to the political whims of Washington, D.C.” On the bright side, if Newsom or Inslee succeeds in making healthcare more affordable and accessible for all with a new model, it will probably be replicated one by one in other states. That’s why I’m hopeful. In 2004, the Canadian Broadcasting Corp. conducted an exhaustive nationwide poll to select the greatest Canadian of all time. The top-10 list included Wayne Gretzky, Alexander Graham Bell and Pierre Trudeau. No. 1 is someone most Americans have never heard of: Tommy Douglas. Douglas, a Baptist minister and left-wing politician, was premier of Saskatchewan from 1944 to 1961. Considered the father of Canada’s health system, he arduously built up the components of universal healthcare in that province, even in the face of an infamous 23-day doctors’ strike. In 1962, the province implemented a single-payer program of universal, publicly funded health insurance. Within a decade, all of Canada had adopted it. The United States will presumably, sooner or later, find a model for healthcare that suits its values and its needs. But 2019 may be a time to look to the states for ideas rather than to the nation’s capital. Whichever state official pioneers such a system will certainly be regarded as a great American. This story originally appeared on Kaiser Health News, and also ran in the New York Times. Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
Traveler Tips: Is The PT Compact License Worth It For Travel PT?

By Stephen Stockhausen, PT, DPT, OCS, Contributing Writer, Founder of PT Adventures Having the freedom to take different jobs in various parts of the country is by far the best, and the most obvious, perk of being a travel physical therapist. But it comes at a cost of the occasionally arduous task of obtaining a new state license. There are the jurisprudence exam, state license fee, FSBPT test score verification fee, and license verification letters—with subsequent fees that need to be sent to any state you have ever held a license. Whew! That’s exhausting just to type out let alone piece together and mail off. Oh, and then you have to wait anywhere from two to six months to find out if you’re new license has been granted or not. But fear not—the Physical Therapy Compact license is designed to fix all of that! In case you haven’t heard about the Physical Therapy Compact license here is a quick summary. Enacted in 2017, the Physical Therapy Compact Commission was created to provide a vehicle for improved interstate license accessibility while maintaining the safety of the public consumer as set forth by each state’s practice act, according to their website. The PT Compact Commission has since built up an impressive list of 21 states willing to recognize the validity of physical therapist and physical therapist assistant licenses from other participating states. The first privileges were then officially granted in July of 2018. While all 21 states have passed legislation to be members, not all states are currently issuing compact license privileges at this time and are still resolving internal issues—or just dragging their feet. At the time of this writing, nine states are active participants in the compact license process, with more joining every month! Pros and Cons of the Physical Therapy Compact License for travelers Pros: Therapy privileges can be granted in minutes rather than months Once you take the jurisprudence exam for your new state—often completed online—and pay the necessary fees, you are eligible to begin working in the new state Low Fees The fees involved with the new PT Compact are very minimal compared to sending out license verification fees for each state you have ever had a license. $45 goes to the PT Compact Commission, and then each state has their own fee. Most range from $45-60, with the exception of Mississippi at $150. (Come on, Mississippi!) One set of Continuing Education Units (CEUs) to manage Since you do not have a full state license in every state that you obtain privileges for, you do not have to maintain their Continuing Education Units. The only set of CEUs that you absolutely must follow is that of your home state. Gone are the headache-inducing hours of cross-checking CEU dates with license expiration dates! Renewal This is one of the coolest aspects of the Compact system. 60 days before your home license expires they will email you a reminder. Once you renew your license at home, the Compact will automatically notify you that you are eligible to renew your Compact privileges as well, typically within a week. Responsive Admin Team When I was doing research for this article, I had a few questions that I could not find on their website. Opting to call instead of email, I was quickly connected with the lead administrator who thoroughly answered my questions and was exceedingly friendly. This was a pleasant surprise compared to the typical experience I have come to expect when dealing with licensing staff at the various states I have worked. Telehealth? While not entirely applicable to the traveler, based on the language written into the Compact it appears that Compact privileges can also be used to treat remotely via telehealth. In a burgeoning field, this is super exciting news! Especially for the therapist looking to mix in some patient care in a state where they previously worked as a traveler or will soon work as a traveler. Instead of being limited to one license per job, multiple licenses can be utilized all at once depending on the patient’s location, independent of where the PT is located. Cons: Few states fully participating Obviously, if your home state is not a participant you are fully excluded from the entire process… bummer. For those of you who are fortunate enough to have a home state proactive enough to join up, your options for states to travel to may be slim pickings. Currently, only nine states are fully active. On the positive side they are some pretty cool states. Oregon, Utah, New Hampshire and North Dakota all have some great outdoor experiences. Texas Tennessee, Missouri and Mississippi all have some killer food and Southern hospitality. As for Iowa…well, Field of Dreams is there. That’s something! There are 11 other states on the doorstep to full participation so check the site often to see if your home state or dream location is up and running. When you renew your home license you have to renew ALL of your Compact Privileges This will negatively impact folks living in a home state that requires yearly license renewal. These therapists will now have to pay all of the Compact fees again as well as fees to the state where they are working. Now, compared to paying all of the other fees typically involved in maintaining multiple licenses, this could still end up saving you money, but you will have to do the math on your specific situation to be sure. Overall the PT Compact License is—or is going to be—a huge improvement in the logistics of being a travel therapist, especially if more states get involved. If every state were to join the Compact, it would mean one license to worry about, one set of CEUs, and only paying fees to the states where you are actively working. Stephen Stockhausen is a doctor of physical therapy, a traveler, and a founder of PT Adventures—a blog created with his wife Ellen to help travel PTs take control of
Travel Healthcare As A Pair: Getting Creative When The Market is Tricky
By Alex McCoy, Contributing Writer, Owner of Fit Travel Life My husband Keaton and I are lucky enough that we both have careers that allow us to travel as a pair. I am a registered nurse and he is a physical therapist, so we are both able to work 13-week contracts throughout the country. We have been doing this for about 18 months and have managed to find contracts together about half of the time we have traveled. Even if you don’t have a spouse who can travel, many people choose to travel with a friend who is also a travel nurse. Not only does this help with loneliness on the road, but it cuts back on the cost of living and some of the work that has to be done when you move to each assignment. If you travel as a pair it can be a little trickier to find jobs that work for both of you at the same time in the same area. In the past 18 months, we have gotten a little creative, but we have managed to make it work and have some great ideas for anyone else looking to travel as a pair. Look for jobs in larger metropolitan areas. While some rural assignments offer big money based on location, the job concentration will be much lower. We have had much better luck if one person takes a job in a big city and then the second person works on finding something in that area. Plus, jobs are more likely to pop up for later start dates throughout the duration of the first person’s contract (more on that later). Be willing to have a longer commute. Many large metropolitan cities come with the price of heavier traffic. Keaton and I have each had to commute up to 1 hour each way to find contracts in a similar area. Whether it is heavy traffic or long distance, commute time could very well be an issue you have come up when trying to find jobs in the same location. Have a plan for if one person’s contract falls through. We always pick our housing based on one person’s income. Because contract cancellations are an unfortunate part of working as a traveler, we want to know we can survive even if one of us gets cut from a job. Similarly, if you travel with a friend, make sure and have a plan or a good chunk of savings in case you lose your job while on location. Look for start dates no more than 3-4 weeks out. A few times one of us has jumped on a great-paying contract early only to find the market drying up for the other person. The travel market is so hard to predict, so you may not be able to guarantee jobs for both individuals if you look too far in advance. For example, the Phoenix market was great back in the fall, but by the time we got here in the winter, physical therapy jobs for my husband had dried up and he has had to get a little creative with finding work. Which brings me to my next point… Don’t be afraid to think outside the box for jobs. Even if you can’t find a contract, that doesn’t mean there aren’t facilities in need nearby. I was able to sign up for per diem flu shot clinics in Georgia, and my husband found a per diem agency locally in Phoenix. Many hospitals choose to use local agencies first, so you may have luck reaching out to them directly once you are in town. Some places will even hire you directly knowing you’re short term because ultimately it saves them more money than hiring a traveler through a company. While traveling with a friend or spouse may take a little more leg work, it sure is nice when you get hit with a little bit of homesickness or loneliness. Knowing you have a roommate or companion to lean on is always a great source of comfort when dealing with the stress of changing jobs and adjusting to a new floor. Be sure to be open and honest with your recruiter about your goals are if you are traveling as a pair. It is even more beneficial if you share a recruiter, but for many companies that won’t be possible if you are different professions or specialties. Also, keep in mind my previous advice about working with more than one company, as it will be especially helpful if you need to try and match specific locations with your travel partner. Alex McCoy currently works as a pediatric travel nurse. She has a passion for health and fitness, which led her to start Fit Travel Life in 2016. She travels with her husband, their cat Autumn and their dog, Summer. Alex enjoys hiking, lifting weights, and trying the best local coffee and wine.
5 Things They Don’t Tell You About Travel Nursing

By Alex McCoy, Contributing Writer, Owner of Fit Travel Life Now that the new year is officially in full swing there are a lot of people evaluating their life. Where do I want to be in five years? Am I working in a career that I love? What if now is the best time to take that leap I have been considering for a while? If you have been considering working in travel nursing for any amount of time I want to preface by saying I highly recommend this career path. My experience as a whole has been positive and to anyone considering travel nursing, I would say go for it. However, as with any positive thing, there are the inevitable negative aspects that come along with it. Getting into the travel nursing world can be daunting, and being unprepared is the worst thing you can do if you want to enjoy your work as a traveler. I feel that being upfront and honest about some of the common struggles travelers face is the best way for new travelers to be prepared to manage these stressors as they come along. Here are the top five downsides to traveling that I feel all travel nursing newbies should be prepared for: 1. There is a lot of behind the scenes work to get started in travel nursing. Before you can even submit to jobs, you must have references and an updated resume ready to go. In addition, you have to have licenses on hand, locations in mind and have a baseline idea of housing costs before you actually apply. Once you have secured a position, there is usually at least a few hours of credentialing and paperwork to complete. This includes visiting a walk-in clinic for drug screens, updated labs and submitting proof of all prior vaccinations and licenses. 2. There will be upfront expenses before you get your first travel nursing paycheck. Most travel nursing contracts include a form of travel reimbursement—on the first check, that is. This means if you move in the Sunday before a Monday start day, you will not actually receive your first housing stipend or travel money until about 12 days later. Some costs to consider at the start of each assignment include first month’s rent, pet deposits, and travel expenses on the way there. I have had to pay close to $3,000 before actually starting work, so planning ahead for this is key. 3. Each state has different renewal requirements you have to monitor. To make yourself more valuable as a travel nurse you will want more than one state license. If your home is in a compact state this is great, but a lot of the destination states are not part of the compact (Hawaii and Alaska in particular). After the leg work of getting the license is complete, you then have to maintain said license. Each state has different guidelines and fees for renewals and you will have to check the individual boards to make sure you stay on top of these. 4. Loneliness is a real problem in travel nursing. A more obvious downside to travel nursing is lack of in-person connections in each area you live. You may make friends on assignment but there is always an awkward period at the beginning where you don’t necessarily have people to hang out with outside of work. While there are many ways to combat this loneliness, it is also helpful to be aware of it so you can meet it head-on. This is a normal feeling and it is okay to be lonely, but have some plans in place to deal with these emotions. Call a friend, go to a workout class, or just go for a walk if you are feeling especially down about a lack of personal interactions. 5. If you decide to switch companies, all of that hard work has to be done a second time. Working with multiple companies is almost inevitable in travel nursing, but that doesn’t mean it is easy to coordinate. Each time you decide to submit for a contract with a company you haven’t worked with, you will have to re-submit your resumes, references and paperwork. The best way to handle this is to get organized at the start. Keep a folder of all your personal identification, license copies, and vaccination records. In the event that you have a company pay for a vaccine, TB test or physical, always request copies of these records in case you work with a different company for your next contract. By keeping your files up to date you can simply send all of your paperwork over in a matter of a few clicks each time you need to establish a contract with a new company. This can all be a bit of a downer, but I would not change my choice to work in travel nursing for anything. The people I have met and the experiences that came as a result of this career are without a doubt worth all of the extra work and planning. By being prepared and knowing what to expect you can have a more positive experience as a traveler and minimize the anxiety that comes along with this career. Expect the unexpected, plan for bumps in the road, and just be thankful when you don’t have to make use of those plans when everything goes smoothly. Alex McCoy currently works as a pediatric travel nurse. She has a passion for health and fitness, which led her to start Fit Travel Life in 2016. She travels with her husband, their cat Autumn and their dog, Summer. Alex enjoys hiking, lifting weights, and trying the best local coffee and wine.
After Bitter Closure, Rural Texas Hospital Defies The Norm And Reopens (KHN)
By Charlotte Huff, Kaiser Health News Five months ago, the 6,500 residents of Crockett, Texas, witnessed a bit of a resurrection — at least in rural hospital terms. A little more than a year after the local hospital shut its doors, the 25-bed facility reopened its emergency department, inpatient beds and some related services, albeit on a smaller scale. Without a hospital, residents of Crockett, located 120 miles north of Houston, were 35 miles away along rural roads from the next closest hospital when a medical crisis struck, said Dr. Bob Grier, board president of the Houston County Hospital District, which is the county’s governmental authority that oversees Crockett, a public hospital. “Someone falls off the roof. A heart attack. A stroke. A diabetic coma. Start naming these rather serious things and health care is known for its golden hour,” he said. The late-July reopening of the newly named Crockett Medical Center makes it a bit of a unicorn in a state that has led nationally in rural hospital closures. Since January 2010, 17 of the 94 shuttered hospitals have been in Texas, including two that closed in December, according to data from the University of North Carolina’s Cecil G. Sheps Center for Health Services Research. But Crockett’s story also reflects some of the challenges faced by rural hospitals everywhere. Board members frequently have limited background in health care management and yet are responsible for making financial decisions. Add to that mix a Lone Star State resistance to raising local property taxes. An effort to increase the county’s 15 cents per $100 property valuation for the hospital district has been defeated twice since the hospital closed. And a small rural hospital like Crockett’s has “no leverage” when negotiating reimbursement rates with insurers, Grier repeatedly points out. The tough reality is that too many rural hospitals in Texas and elsewhere, when negotiating with insurers and other financial players, “are almost always negotiating from weakness and sometimes from literally leaning out over the edge of the [survival] cliff,” agreed Dr. Nancy Dickey, executive director of the A&M Rural and Community Health Institute at Texas A&M Health Science Center. Rural communities must think more creatively about how to meet at least some of their health needs without a traditional hospital, whether it’s forming partnerships with nearby towns or expanding telemedicine, Dickey said. “There is little doubt in my mind that many of these communities are going to see their hospitals close,” she said, “and are not going to be able to make an economic case to reopen them.” The A&M institute, which in December published a report looking at these challenges for three Texas communities, recently landed a $4 million, five-year federal grant to help rural hospitals nationwide keep their doors open or find other ways to maintain local health care. Demographics And Decisions The financial headwinds have been particularly fierce in Texas, one of 14 states that has not expanded Medicaid eligibility after the passage of the Affordable Care Act. “That makes a huge difference,” said John Henderson, chief executive officer of the Texas Organization of Rural & Community Hospitals, known in Texas rural circles as TORCH. “But that doesn’t change the reality that we aren’t going to do it.” Leading up to the state’s biennial legislative session, which begins in January, rural leaders are making the case that state legislators need to take steps to bolster the state’s 161 rural hospitals, starting with rectifying underpayments for Medicaid patients. As the state’s program has transitioned to managed care, over time reimbursements have shrunk to the point that rural hospitals are losing as much as $60 million annually, according to TORCH officials, who cite state data. They also support a congressional bill, HR 5678, that would make it easier for rural hospitals to close their inpatient beds but retain some services, such as an emergency room and primary care clinic. Under current federal regulations, facilities that make such a move are no longer considered a hospital and can’t be reimbursed by Medicare and Medicaid at hospital rates, which are often higher than payments to clinics or individual doctors. Those lower rates make it harder for stripped-down facilities to keep up their operations, said Don McBeath, TORCH’s director of government relations. Crockett’s hospital, then called Timberlands Healthcare, abruptly shut down in summer 2017 after just a few weeks’ notice from its management company, Texas-based Little River Healthcare. Little River, which was also the subject of an analysis by Modern Healthcare that showed several of its hospitals engaged in unusually high laboratory billing for out-of-state patients, has since filed for bankruptcy. Two other rural hospitals affiliated with Little River closed their doors in December As it struggled to stay open, Crockett’s hospital had been treating a population that was increasingly poor and aging, according to Texas A&M’s report. The researchers describe in the report — Crockett is “community 1” among three communities featured — that the hospital was overstaffed with more than 200 employees given its daily average census of three hospitalized patients. Also, they wrote, board members should have more closely questioned the management company. The board said they were given data at each meeting, “but that data did not suggest the imminent demise of the hospital,” the report’s authors wrote. Fighting The Closure Tide Leaders in Crockett tried to capture the interest of other hospital systems to reopen and manage the facility, without success, Grier said. Along with staffers losing their jobs, the community knew it would be more difficult to persuade people to relocate or retire to the area without a hospital nearby, he said. Every weekday at noon for weeks on end, a small group of two to 20 people gathered beneath the hospital’s front portico to pray for some avenue to reopen, Grier said. Then, as the odds looked increasingly long, they got a call out of the blue from two Austin-based doctors. “I feel God was involved,” Grier said. “They have told us that they were looking for some
Healthcare Is Where The Jobs Are. But What Kind Of Jobs? (KHN)

By Rachel Bluth, Kaiser Health News More Americans are now employed in healthcare than in any other industry. The Bureau of Labor Statistics, which tallies job creation, says that for most of this year the health sector outpaced the retail industry. Only government, on all levels, employs more people. One of the consistent features of the BLS reports is that healthcare has reliably added thousands of jobs to the economy each month. November was no different. The healthcare industry created 32,000 jobs, adding to the 328,000 healthcare positions created since early 2017. But what kinds of jobs? Were they highly paid doctors and hospital executives or were they positions on the other end of the pay scale, such as nursing home aides and the people who enter data for billing in hospitals and clinics? It’s hard to know for sure, because the BLS monthly data measure industries not occupations and what information it does have on occupations is overly broad. For instance, it says hospitals accounted for about 13,000 jobs in November. Another 19,000 jobs were for “ambulatory” care, which is a broad term for services delivered outside of hospital systems, like in clinics and private doctors’ offices. But another set of BLS data offers additional insights. Every two years, BLS puts out a wonky set of numbers called “industry-occupation matrices,” which more finely slices job categories and predicts which will grow or shrink over the next 10 years. The most recent, from 2016, still provides a pretty accurate snapshot, according to Joanne Spetz, a professor at the University of California-San Francisco’s Institute for Health Policy Studies. Registered nurses are the fastest-growing occupation. They account for more than 25 percent of jobs in hospitals. If that share remained the same last month, 3,289 of the new hospital jobs added in November went to RNs. [protected-iframe id=”afd374bef04176b4120013d3f73733ab-7618883-99279322″ info=”//datawrapper.dwcdn.net/XoirU/5/” width=”100%” height=”500″ frameborder=”0″ scrolling=”no”] It’s likely that many of the hospital jobs went to medical assistants, who currently make up only 1.5 percent of the industry. Medical assistants are usually the people taking your vitals and helping the doctor take notes. The BLS expects about a 16 percent increase in these jobs in the next decade. “There will be a fair amount of growth in physician and surgeon employment in the next decade, but so many more medical assistants than physicians,” Spetz said. The national median pay of a registered nurse is $70,000 a year, according to more BLS data. For medical assistants, it is $32,480. Doctors’ median pay is more than $200,000. Far more of those medical assistants found work outside the hospital in the ambulatory sector: almost 1,300. There is also a good chance that in these ambulatory settings many of the newly created jobs were filled by non-medical staff. As of 2016, fewer than 30 percent of staff in ambulatory settings were workers whom Spetz calls “paper pushers.” If the trend held up, around 5,700 of the hires in November, or 30 percent of ambulatory jobs, fall into these categories. These jobs can pay as much as medical assistants. The BLS says the median income of “medical record and health information technicians” is about $39,000 a year. BLS is predicting around a 20 percent increase in “information and record clerks” and another 22 percent increase in “secretaries and administrative assistants.” But the idea that hospitals and doctors’ offices are hiring only lower-paid support staff might be overblown. The BLS figures “healthcare practitioners and technical occupations” still make up more than 37 percent of the ambulatory industry, and “health diagnosing and treating practitioners” are almost 23 percent. So nearly 70 percent of ambulatory hires last month were probably physicians or other skilled professionals like registered nurses, licensed practical nurses, social workers and personal care aides. “What we have seen over the past couple years is with the job growth in health it is not dominated by back office,” said Ani Turner, an economist who focuses on health sector labor trends with Altarum, a nonprofit health research and consulting organization. Another thing hiding in the numbers? A dissipating distinction between ambulatory and hospital care. Traditionally, hospital jobs were pretty straightforward; they referred to the doctors, nurses and support staff who worked in hospitals. But as business models shift, more care is given outside of hospital walls, something not reflected in employment numbers that split health into two distinct categories. Employees who staff the clinics, surgery centers, labs and imaging centers run by hospitals are counted as hospital staff, Turner said, though they work in outpatient settings. So those 13,000 new hospital jobs the BLS cited last month may not reflect real-world trends about where hiring happens. “Whether in physicians’ offices, free-standing clinics or hospital outpatient clinics, you’ll see it as the two separate settings, but the same trend,” Turner said. This story originally appeared on Kaiser Health News. Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
Virginia Medicaid Expansion Enrollment Exceeds Projections

State officials had estimated 300,000 newly eligible Virginians would sign up for Medicaid coverage in the first 18 months of expansion, which takes effect on Jan. 1, but that estimate has increased based on the current pace of enrollment. As of Thursday morning, 140,643 adults now eligible for coverage under the expansion have enrolled in Medicaid, said Christina Nuckols, a media relations manager with the Virginia Department of Medical Assistance Service. State officials updated their estimate to 375,000 total enrollments by July 2020. That’s still 25,000 short of the 400,000 estimated Virginians who fall within the coverage requirements. Under the Affordable Care Act, states that expand Medicaid allow coverage for people with incomes up to 138 percent of the federal poverty level, which is $16,750 a year for a disabled person or able-bodied adult and $28,700 for a family of three. Virginia residents, find out eligibility requirements and how to enroll in Medicaid here >> A combination of automatic enrollments and streamlined enrollment processes for residents the state already knew were eligible—like those who receive Supplemental Nutrition Assistance Program benefits—are some of the reasons why the pace of signups have exceeded expectations, according to a Washington Post report. As part of the expansion, the federal government is expected to cover 90 percent of the cost of the program, to the tune of $2 billion annually. Virginia will foot its portion of the expansion costs through two new hospital taxes, which are expected to raise $590 million in two years, $248 million of which will be used to boost the reibursment rate for acute care facilities that treat Medicaid patients. The impact on travel healthcare in Virginia Even with less than one month until thousands of new potential low-income patients gain insurance coverage, Virginia hospitals are more worried about handling current needs than worrying about future patient loads, said Imran Chaudry, a senior client advisor for LiquidAgents Healthcare. “In the Richmond area, I can tell you from the feedback I’ve gotten that every hospital is still slammed,” Chaudry said. “I’ve tried talking to all of my…clients about the Medicaid expansion, but nobody is talking about that because they are so wrapped up in their day-to-day.” Job orders for travelers in the state have increased significantly since the start of November, Chaundry said, from around 100 positions to almost 200 open positions as of Dec. 5. Most of the market growth has occurred in the northeast and eastern portions of the state, around the greater Richmond region, Chaundry said. View current Virginia travel healthcare openings on StaffDNA >> Bon Secours Health System, the largest healthcare provider in the Richmond region, merged with Cincinnati-based Mercy Health in September. The merger is expected to boost services for Bon Secours in three markets including the Hampton Roads Health system near the state’s coast, according to a Modern Healthcare report. Both the Richmond region and the Hampton Roads region serve large populations of low-income residents, which could result in a wave of demand for travelers once newly covered Medicaid patients gain coverage in January. Studies have shown that low-income populations prefer using hospital emergency departments instead of primary care doctors for their around-the-clock availability and ease of use.
At Least 40 Hospital Labor Disputes Made Headlines In 2018

At least 40 hospital labor disputes ranging from heated contract bargaining debates to extended strikes occurred in 2018, according to a recent analysis by Healthcare Dive. Here are the key takeaways from hospital labor disputes in 2018. Most of the disputes occurred in heavy union or non-“right to work” states. Based on Healthcare Dive’s analysis, most of the hospital labor disputes that garnered media attention occurred in the Northeastern and Western regions of the U.S. California had the most labor disputes on the West Coast at 13, while Pennsylvania had the most in the Northeast with seven. California and many of the states in the Northeast have the highest union participation in the country. New York, which has the highest number of union-affiliated employees in the country at 25.3 percent according to the Bureau of Labor Statistics, had two major disputes this year. Florida and Texas were the only two states with major labor disputes in 2018 that are not in the top 20 states in terms of union members. Both states were involved in a potential strike at 15 HCA-owned facilities in September, but the facilities involved reached an agreement in October, according to a National Nurses United press release. Nurses were involved in the most labor disputes Out of the 40 healthcare labor disputes listed in Healthcare Dive’s analysis, 21 of them were led primarily by nurses and nurse unions, 18 had a mix of medical and non-medical staff, and one was led by healthcare technicians. Unsafe staffing, low or uncompetitive wages and lack of benefits were cited as the primary concerns for most of the labor disputes. July was the busiest month for healthcare labor disputes in 2018 At least eight major healthcare labor disputes occurred in July this year across the country, according to the analysis. Among those was a three-day strike by workers in Rhode Island against the Providence-based healthcare system Lifespan. Picketers at MountainView Hospital in Las Vegas, Nevada and Corpus Christi Medical Center in Corpus Christi, Texas, would later vote to approve a strike at 15 HCA-affiliated hospitals in September. To see Healthcare Dive’s full analysis of labor disputes in 2018, click here. You can find our strike and protest coverage for 2018 in the list below: Union nurses vote to authorize strike at Michigan Medicine (Sept. 21) National Nurses United members at 15 hospitals authorize strike (Sept. 5) Rhode Island healthcare workers strike begins; Lifespan spends $10M on temp staff (July 23) Kaiser healthcare workers plan new round of protests at California facilities (May 1) Kaiser proposes change to national labor partnership amid union fractures, continued protests (May 15)
