2018 Election: Healthcare Issues Travelers Should Watch

One of the benefits of being a travel healthcare professional can be the opportunity to avoid hospital politics, but national politics are much harder to ignore. Many hot-button healthcare issues decided at the polls can have a direct impact on the travel healthcare job market, both positive and negative, and the 2018 midterm election on November 6 is no exception. Below, we’ve provided brief summaries on ballot initiatives across the country that could have tangible effects on the travel healthcare market. For those who need more information on when, where and how to vote in the midterms, check out our 2018 midterm election voting FAQ. 2018 Election Healthcare Issues California Prop 4, Children’s Hospital Bond Initiative Proposition 4, also known as the Children’s Hospital Bond Act Fund, would authorize $1.5 billion in bonds that would be used to award grants to children’s hospitals for construction, expansion, renovation, and equipment projects. With interest over 35 years, the bond’s total cost would be $2.9 billion. The bonds would be repaid over a period of time from the state’s General Fund, according to the state website. According to Ballotpedia, the $1.5 billion would be distributed as follows: 72 percent ($1.08 billion) to eight nonprofit hospitals providing comprehensive services to high volumes of children eligible for governmental programs and children with special health needs eligible for California Children’s Services. 18 percent ($270 million) to five University of California general acute hospitals, including the University of California, Davis Children’s Hospital; Mattel Children’s Hospital at University of California, Los Angeles; University Children’s Hospital at University of California, Irvine; University of California, San Francisco Children’s Hospital; and University of California, San Diego Children’s Hospital. 10 percent ($150 million) to public and private hospitals that provide pediatric services to children eligible for California Children’s Services Why this is important for travelers If approved by Californa voters, the massive cashflow could provide many positive benefits for both children’s facilities and travelers. Hospitals would be able to update, renovate or construct new units, which could improve quality of care for patients, improve the working environment for healthcare professionals and potentially provide staffing opportunities for travelers. Idaho Proposition 2, Medicaid Expansion Initiative Idaho Medicaid expansion advocates successfully petitioned and gathered 75,314 verified signatures to add a Medicaid expansion measure to the ballot. The petition met both state requirements to qualify the ballot measure, gathering at least 56,192 verified signatures that represented at least 18 of Idaho’s 35 legislative districts. An expansion would allow Idaho residents under 65 and earning incomes at 138 percent of the national poverty level to apply for Medicaid insurance. About 62,000 Idahoans would qualify for this coverage. Expansion would also bring in $105 million in costs to the state over 10 years and $200 million in savings, according to an independent analysis by The Milliman consulting firm. Why this is important for travelers Studies have shown that hospitals in Medicaid expansion states have not only saved tremendously on uncompensated care costs, but they also have also seen more newly-insured patients coming in for healthcare services. The increased patient needs and loosened revenue streams could result in more opportunities for healthcare travelers. You can read more about this issue in our Medicaid expansion guide. Massachusetts Question 1, Nurse-Patient Assignment Limits Initiative Approval of Question 1 in Massachusetts would establish a set nurse-to-patient ratio across all state hospitals, except during a public health emergency. This measure would also require the limits to be met without a reduction in staff, and would allow the Massachusetts Health Policy Commission to regulate and enforce the initiative, which could result in $25,000 per incident for hospitals that violate the mandated ratios. If approved, Massachusetts would become the second state with mandated nurse-to-patient ratios—currently, California is the only state that has them. According to an independent study by the Massachusetts Health Policy Commission, implementing the mandate would cost from $676 million to $949 million per year. They also estimated possible savings of $34 million to $47 million from reduced hospital length of stay and potential for improved patient care with increased nurse staffing. State hospitals would also need to increase staffing by 2,286 to 3,101 additional full-time equivalent nurses to comply with the mandated ratios, according to the study. Medical-surgical and psychiatric nurses would present the greatest needs for increased staffing. Why this is important for travelers Of all the healthcare initiatives voters will decide on at the polls this fall, Question 1 could have the biggest and most direct impact on travel nurses. Mandated ratios mean more nurse hiring, which also means significantly more opportunities for travel nurses. You can find more information additional details on the impact of this change by checking out our recent coverage of the ballot issue. Utah Utah Proposition 3, Medicaid Expansion Initiative Utah Gov. Gary Herbert signed a bill on March 27, 2018, for partial Medicaid expansion, directing the state to seek federal approval to expand Medicaid to 100% of the federal poverty level. The bill stipulated using the ACA enhanced federal match rate and adding a work requirement for the expansion population. The Center for Medicare and Medicaid Services (CMS) has not approved waivers to access the match rate until Utah approves a full expansion. In the meantime, Utah expansion advocates garnered enough petition signatures to add a competing bill to November ballots that would approve a full expansion. An expansion would provide an estimated 150,000 Utah residents with Medicaid coverage. Why this is important for travelers Studies have shown that hospitals in Medicaid expansion states have not only saved tremendously on uncompensated care costs, but they also have also seen more newly-insured patients coming in for healthcare services. The increased patient needs and loosened revenue streams could result in more opportunities for healthcare travelers. You can read more about this issue in our Medicaid expansion guide. Nebraska Nebraska Initiative 427, Medicaid Expansion Similar to Idaho and Utah, Nebraska advocates have submitted a petition to add a Medicaid expansion initiative to the midterm election ballot. Supporters filed more than 133,000 signatures on July 5 and a large enough majority
EMR Conversions: Appalachian Regional Kicks Off Meditech Upgrade In Kentucky, West Virgina

Appalachian Regional Healthcare (ARH), the largest not-for-profit healthcare system in Southeastern Kentucky, is in need of hundreds of travel nurses over the next several months for a system-wide electronic medical record (EMR) conversion, according to industry reports. View current West Virginia travel nursing EMR conversion jobs on the StaffDNA boards >> Currently, Meditech EMR conversion jobs are open at Beckley ARH in West Virginia and Middlesboro ARH in Kentucky, with more expected through the rest of 2018 and into 2019. As of Oct. 29, all major travel nurse specialties are needed, including medical-surgical, labor and delivery, ER, ICU and more. ARH operates 12 hospitals, 11 home health agencies and multiple clinics, pharmacies and home care stores, most of which are located in Southeastern Kentucky. The healthcare system plans to convert its smallest facilities first, working its way up to 358-bed Hazard ARH sometime in 2019. Travel nurses who apply can expect very quick interviews and offers for these EMR conversion jobs, Oren Lavi with LiquidAgents Healthcare said. View current Kentucky travel nursing EMR conversion jobs on the StaffDNA boards >> “Nurses will have more options to move and extend [on contracts] after these initial EMR assignments are complete, as they will be able to move to other facilities that are converting,” Lavi said. ARH is implementing a new EMR for the first time, upgrading from paper charting to an integrated Meditech charting system. ARH announced their selection of Meditech in 2017, according to an official press release. “We are excited to partner with Meditech in providing ARH an innovative Web EHR that fosters and supports sustainability,” Joe Grossman, ARH’s president and CEO said in a 2017 press release. “With the Web EHR, our clinicians will have seamless integration across the continuum, improved productivity, and the sophisticated tools to improve the quality and safety of care delivered to our communities.” What to know about working in Kentucky Kentucky is a favorable state for travelers looking to save money as the cost-of-living is low, according to the U.S. Bureau of Economic Analysis. In a 2018 BEA report, Kentucky ranked as the 5th most affordable state in the U.S., thanks to some of the lowest apartment and home rental rates in the country. Nurses can also use a compact license to work in Kentucky. The state joined the enhanced Nursing Licensure Compact this year, along with more than 20 other original NLC states.
Nurses at 2 Arizona hospitals vote to join national union

Nurses from St. Joseph’s Hospital and St. Mary’s Hospital in Tuscon, Arizona voted Friday to unionize, joining the National Nurses Organizing Committee and National Nurses United, according to a press release. About 550 nurses at St. Joseph’s and 450 at St. Mary’s are now represented by Tenet Health division of the national union, swelling the group’s membership total to more than 6,000 registered nurses and 14 Tenet facilities across four states. Both hospitals are part of the Carondelet Health Network in Tucson, which is owned by Tenet Health Corporation based out of Dallas, Texas. In a 293-110 vote, 73 percent of the nurses at St. Joseph’s voted in favor of unionizing and 221-85, or 72 percent, voted in favor at St. Mary’s. Both votes were conducted by the National Labor Relations Board, according to the press release. “I am so excited that we will now be able to advocate much more effectively for our patients,” Lowella Choate, a neuro ICU nurse at St. Joseph’s Hospital said in a press release. “I look forward to all that we can achieve by standing together with the 6000- RN-strong NNU Tenet Division at 14 Hospitals throughout the country.” As Arizona is a right-to-work state, nurses at the hospitals are not required to join the union as a condition of employment and they don’t have to pay union dues even if actions by the union benefit them. Carondelet Health Network officials told the Arizona Daily Star they would respect the nurses’ decisions and will work with them to reach a “mutually beneficial collective bargaining agreement.” Nurses at the hospitals will elect a team of colleagues to represent them in talks with hospital officials on a first collective bargaining contract, according to the NNU press release.
EMR Conversions: Meditech Travel Nurse Jobs Available In West Virginia

Beckley ARH Hospital, an acute-care facility located in Beckley, West Virginia, is looking to fill 35 travel nurse needs to help with an upcoming EMR conversion, according to a source with LiquidAgents Healthcare. The hospital is transitioning from paper charting to Meditech as part of an ongoing EMR conversion rollout to all Appalachian Region Healthcare facilities that started in 2017. Contact LiquidAgents Healthcare for more information about these EMR conversion travel nurse jobs in West Virginia >> Currently, 35 positions are available for primarily medical-surgical/telemetry travel nurses, but other specialties are available as well. Days, nights and variable shifts are all available at this time. Nurses with a compact license can now use it for West Virginia, as the state joined the enhanced Nursing Licensure Compact this year. Travelers can still apply for a single-state license, but West Virginia is not a walk-through state so it could take 5-10 business days to process. What travelers should know about Beckley, WV Beckley is one of the largest cities in the state and is one hour south from Charleston, the state’s capital. The city also has one of the lowest cost-of-living ratings in the U.S., with average rents at 36 percent of the national average—or about $570 a month on average for a 1-bedroom apartment—so travelers can potentially save hundreds over the holidays on living expenses.
Healthcare Tops Guns, Economy As Voters’ Top Issue

By Phil Galewitz, Kaiser Health News Healthcare has emerged as the top issue for voters headed into the midterm elections, but fewer than half of them say they are hearing a lot from candidates on the issue, according to a new poll released Thursday. Seven in 10 people list healthcare as “very important” as they make their voting choices, eclipsing the economy and jobs (64 percent), gun policy (60 percent), immigration (55 percent), tax cuts (53 percent) and foreign policy (51 percent). When asked to choose just one issue, nearly a third picked health care, according to the survey by the Kaiser Family Foundation. (KHN is an editorially independent program of the foundation.) Still, midterm elections are traditionally a referendum on the president and his party, and that holds true this year as two-thirds of voters say a candidate’s support or opposition to President Donald Trump will be a major factor in their voting decision, the poll found. Health care was also the top issue chosen overall by voters living in areas identified in the survey as political battlegrounds, although the results varied when pollsters drilled down to political parties. Nearly 4 in 10 Democratic battleground voters and 3 in 10 independents chose health care as their most important issue in voting for Congress. Among Republican voters, immigration was their top issue, garnering 25 percent compared with 17 percent for health care. The poll results in two battleground states — Florida and Nevada — also underscored voters’ interest for keeping the Affordable Care Act’s protections for people with preexisting conditions, one of the most popular provisions in the law. Democrats have made that a key part of their campaign, pointing to Republicans’ votes to repeal the entire law and trying to drive home the message that the GOP’s efforts would strip that guarantee. Nonetheless, Republicans have recently sought to fight back on that issue, promising on the stump and in campaign ads that they understand the need to keep the protections and would work to do that. Nearly 7 in 10 Florida voters said they are more likely to vote for a candidate who wants to maintain the protections for people with preexisting conditions, while 9 percent said they are more likely to vote for a candidate who wants to eliminate these protections. In Nevada, nearly 70 percent of voters also said they wanted the ACA preexisting protections guaranteed. In Florida, where the deadliest mass school shooting in American history took place last February, health care also was the top issue among voters. Twenty-six percent of Florida voters listed health as their top issue. The economy and gun policy tied for the second-biggest issue at 19 percent. The shooting at Marjory Stoneman Douglas High School in Parkland, Fla., left 17 students and staff members dead, spurred massive marches around the country and stirred national debate on gun policy. Florida is traditionally a key battleground state but more so this year with close races for the U.S. Senate and governor’s race hanging in the balance. Nearly half of Florida voters said they are more likely to vote for a candidate who wants to expand Medicaid. Florida is one of 17 states that has chosen not to expand Medicaid under the health law, leaving tens of thousands of its adult residents without health insurance. The Republican-controlled legislature has refused to accept millions of dollars in federal funding to extend the coverage. Two in 10 Democratic voters in Florida said support for a candidate supporting a national health plan, or “Medicare-for-all,” is the most important healthcare position for a candidate to take. Andrew Gillum, the Florida Democratic gubernatorial nominee, has said he would support a national health plan. In Nevada, which also has a key Senate battle, the poll found nearly a quarter of voters said health care was the top issue in their decisions this year, but immigration and the economy were very close behind. Nearly a third of Democrats in Nevada said they are looking for a candidate who supports a single-payer health plan. Just under a third of Republicans in Florida and Nevada said that a candidate’s support of repealing the ACA is the most important health issue when they vote. The poll of 1,201 adults was conducted Sept. 19-Oct. 2. The national survey has a margin of error of +/-3 percentage points. This article originally appeared on Kaiser Health News Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
Massachusetts Voters Split On Mandated Nurse Staffing
With only two weeks left until the Nov. 6 midterm election, Massachusetts voters are split evenly on establishing statewide mandated nurse-to-patient ratios, according to a new poll by WBUR, Boston’s NPR news station. Of the 506 Massachusetts residents surveyed, 44 percent were in favor of mandated nurse staffing, and 44 percent were opposed. The remaining 12 percent said they were undecided. Advocates for the mandate, also known as Question 1, have said establishing mandated nurse staffing ratios will lead to better patient outcomes and improve quality of care. Opponents have said the opposite and also claim mandated ratios will put an expensive burden on state hospitals. Both sides claim nurses fully support them. Both groups have spent a combined total of more than $14 million on competing TV advertisements and campaign initiatives. Because both groups have run similar ad campaigns, voters have had a difficult time figuring out how nurses actually feel about the issue, according to the WBUR report. The pro-mandate group, the Committee to Ensure Safe Patient Care, is sponsored by the Massachusetts Nurses Association. Most of the group’s supporters are nursing unions, labor unions, international labor unions and local community groups, according to their website. The group also earned key endorsements from several local, state and federal representatives, most notably Sen. Elizabeth Warren and Boston Mayor Martin J. Walsh. “Nurses work hard to take care of all of us when it matters the most, and we should do the same for them by establishing standards to ensure they have the help they need to do their job safely,” Senator Warren said in a press release. “I stand with our nurses and support a yes vote on Question 1 in November.” The opposing group, known as the Coalition to Protect Patient Safety, is supported mostly by hospitals, hospitals associations and local chambers of commerce, according to their website. The organization has also earned a handful of endorsements from local mayors, including Waltham Mayor Jeanette McCarthy. An independent study conducted by the state’s Health Policy Commission found that implementing the mandate would cost an estimated $676-949 million per year and potentially save $34-47 million. The study also found that hospitals would need to hire 2,286 to 3,101 additional full-time equivalent nurses to meet the mandate. You can read the full analysis of the study below:
Panama City Hospitals Closed, Evacuating Patients After Hurricane Michael

Panama City’s largest healthcare facilities have mostly shut down in the wake of Hurricane Michael’s impact on Wednesday and began evacuating patients Thursday morning. Gulf Coast Regional Medical Center said the hospital’s ER will remain open, but main hospital services have been suspended. Bay Medical Center Sacred Heart (BMSH) began evacuations at 3 a.m. Thursday morning and moved patients to Sacred Heart Hospital in Pensacola, Florida, Providence Hospital in Mobile, Alabama and St. Vincent Healthcare in Jacksonville, Florida, according to a Twitter post. About 200 patients, including 39 intensive care patients, will be evacuated over a 48-hour period. The hospital said no patients were injured during the storm. “All patients, family members, and staff are safe and patient care will continue until the last patient is transferred,” BMSH CEO Scott Campbell said in a press release. “If patients do not have a family member or other support persons with them at the hospital, we are reaching out to their emergency contacts.” 1 of the County Hospitals (Sacred Heart) aka Bay Medical Center on MLK … Gulf Coast Regional has suffered damage as well. Waiting to hear back from them regarding where my Grandmother is being transported. #hurricanemichael #panamacity pic.twitter.com/m6Rg0bJLOV — L Miller (@ohlizalizaliza) October 11, 2018 The hospital sustained significant structural and water damage, including a section of roof that collapsed in the hospital’s materials management building which damaged items needed for long-term care. The hospital plans to keep the ER open as the generator still has power. “Our staff and physicians have demonstrated extraordinary dedication throughout this crisis, providing exemplary care for our patients,” Campbell said. “This has been a truly noble effort and we are deeply grateful for their sacrifice.”
Hurricane Michael: Florida Panhandle Hospitals Brace For The Storm
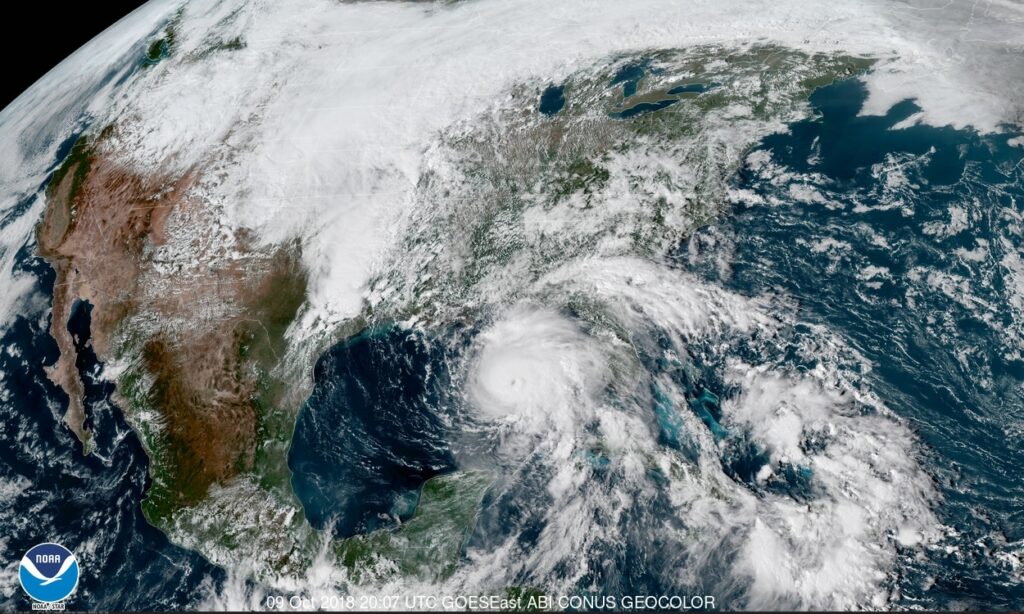
Update, 8:30 a.m. CST, Oct. 10, 2018 After gathering speed and intensity, Hurricane Michael is tearing towards the Florida Panhandle and increased in strength Wednesday morning. As of 8 a.m. CST, Michael was upgraded to a Category 4 hurricane with top sustained winds of 145 mph. Forecasters have said Michael could be the strongest storm to hit the Florida Panhandle in history, affecting nearly 30 million people in the Southeast. New forecasts expect Michael to make landfall Wednesday afternoon. Along with devastating wind speeds, storm surge predictions also increased to 14 feet and forecasters warn of flash flooding in Florida, southern Alabama and Georgia. Florida Gov. Rick Scott and emergency response officials have advised any residents who have not already evacuated need to hunker down, as it’s too late to leave the area. “The time for evacuating along the coast has come and gone,” Gov. Scott said in a Twitter post. “First responders will not be able to come out in the middle of the storm. If you chose to stay in an evacuation zone, you must SEEK REFUGE IMMEDIATELY.” You can find online resources for emergency preparedness and help here: Find open shelters here: https://www.floridadisaster.org/shelter-status/ Free housing for evacuees and disaster responders available through Airbnb: https://www.airbnb.com/welcome/evacuees/hurricanemichael Report significant debris from the storm: https://survey123.arcgis.com/share/466259a6f3fc41e58bb3f651e59e3bd1 App for emergency updates on the storm: http://fpbs.org/get-emergency-info-on-free-florida-storms-mobile-phone-app/ Find out current traffic conditions: https://fl511.com/App Original Story Hurricane Michael, a major hurricane with winds up to 120 mph, is expected to make landfall Wednesday afternoon near Panama City, covering most of Florida’s Panhandle region, according to current hurricane models. The National Hurricane Center expects life-threatening storm surge—up to 12 feet in some areas—along the coast of the Florida Panhandle, Big Bend and Nature Coast regions. Hurricane-force winds from Michael will extend across parts of the Panhandle, southern Georgia and southeast Alabama. Unlike Hurricane Florence in September which stalled on the Carolina coast dumping record-breaking rainfalls, Michael is expected to move quickly through the Panhandle and curve northeast, moving through Georgia by Thursday afternoon. The storm could also intensify to a Category 3 hurricane by the time it makes landfall, carrying winds of up to 130 mph. Florida Gov. Rick Scott declared a pre-landfall state of emergency for 35 Florida counties to secure federal assistance and encourage residents to evacuate before the storm hits. Scott also activated 2,500 National Guard members for storm response, he said during a press conference Tuesday. Florida health officials communicated with healthcare facilities and nursing homes Monday afternoon to prepare for the storm, Scott said. After Hurricane Irma hit last year, 14 people died in South Florida when a nursing home lost power and air conditioning. “The Florida Department of Health has five ambulance strike teams and 35 special needs shelter teams ready to deploy,” Scott said. “The expectations are: If you’re responsible for a patient, you’re responsible for the safety of that patient through this entire storm.” As of Tuesday afternoon, several healthcare facilities in the path of the storm activated emergency response procedures, canceling or rescheduling outpatient and elective procedures. Some facilities in the Tallahassee area are monitoring the storm before activating emergency response declarations. Flowers Hospital in Dothan, Alabama is closing all of outpatient departments on Wednesday, according to a WDHN report. In response to the storm, the Department of Health issued an emergency order allowing healthcare professionals with a valid, unrestricted and unencumbered license in any state, territory, or district to render services in Florida during a 30-day period, according to Gov. Scott’s website. Florida became a compact nursing license state this year but does not normally allow for quick temporary licenses. The Florida Board of Nursing office, located in Tallahassee, will be closed until Thursday, according to their voicemail message. Travelers entering the state should be aware that major highways designated as evacuation routes could be congested with evacuees and could affect their access to locations along the Panhandle. Hurricane Safety Checklist Regardless of where you are located or if you’re working at a hospital during the storm, your first priority is to have a disaster plan in place to protect yourself and your family in a time of crisis. The American Red Cross has provided a hurricane safety checklist that has everything you can do to prepare for the storm and respond to the aftermath. We’ve provided a PDF of the checklist below, but you can also download or view it here: Hurricane Checklist
Spurred By Convenience, Millennials Often Spurn The ‘Family Doctor’ Model

By Sandra G. Boodman, Kaiser Health News Calvin Brown doesn’t have a primary care doctor — and the peripatetic 23-year-old doesn’t want one. Since his graduation last year from the University of San Diego, Brown has held a series of jobs that have taken him to several California cities. “As a young person in a nomadic state,” Brown said, he prefers finding a walk-in clinic on the rare occasions when he’s sick. “The whole ‘going to the doctor’ phenomenon is something that’s fading away from our generation,” said Brown, who now lives in Daly City outside San Francisco. “It means getting in a car [and] going to a waiting room.” In his view, urgent care, which costs him about $40 per visit, is more convenient — “like speed dating. Services are rendered in a quick manner.” Brown’s views appear to be shared by many millennials, the 83 million Americans born between 1981 and 1996 who constitute the nation’s biggest generation. Their preferences — for convenience, fast service, connectivity and price transparency — are upending the time-honored model of office-based primary care. Many young adults are turning to a fast-growing constellation of alternatives: retail clinics carved out of drugstores or big-box retail outlets, free-standing urgent care centers that tout evening and weekend hours, and online telemedicine sites that offer virtual visits without having to leave home. Unlike doctors’ offices, where charges are often opaque and disclosed only after services are rendered, many clinics and telemedicine sites post their prices. A national poll of 1,200 randomly selected adults conducted in July by the Kaiser Family Foundation for this story found that 26 percent said they did not have a primary care provider. There was a pronounced difference among age groups: 45 percent of 18- to 29-year-olds had no primary care provider, compared with 28 percent of those 30 to 49, 18 percent of those 50 to 64 and 12 percent age 65 and older. (Kaiser Health News is an editorially independent program of the foundation.) A 2017 survey by the Employee Benefit Research Institute, a Washington think tank, and Greenwald and Associates yielded similar results: 33 percent of millennials did not have a regular doctor, compared with 15 percent of those age 50 to 64. “There is a generational shift,” said Dr. Ateev Mehrotra, an internist and associate professor in the Department of Health Care Policy at Harvard Medical School. “These trends are more evident among millennials, but not unique to them. I think people’s expectations have changed. Convenience [is prized] in almost every aspect of our lives,” from shopping to online banking. So is speed. Younger patients, Mehrotra noted, are unwilling to wait a few days to see a doctor for an acute problem, a situation that used to be routine. “Now,” Mehrotra said, “people say, ‘That’s crazy, why would I wait that long?’” Until recently, the after-hours alternative to a doctor’s office for treatment of a strep throat or other acute problem was a hospital emergency room, which usually meant a long wait and a big bill. Luring Millennials For decades, primary care physicians have been the doctors with whom patients had the closest relationship, a bond that can last years. An internist, family physician, geriatrician or general practitioner traditionally served as a trusted adviser who coordinated care, ordered tests, helped sort out treatment options and made referrals to specialists. But some experts warn that moving away from a one-on-one relationship may be driving up costs and worsening the problem of fragmented or unnecessary care, including the misuse of antibiotics. A recent report in JAMA Internal Medicine found that nearly half of patients who sought treatment at an urgent care clinic for a cold, the flu or a similar respiratory ailment left with an unnecessary and potentially harmful prescription for antibiotics, compared with 17 percent of those seen in a doctor’s office. Antibiotics are useless against viruses and may expose patients to severe side effects with just a single dose. “I’ve seen many people who go to five different places to be treated for a UTI [urinary tract infection] who don’t have a UTI,” said Dr. Janis Orlowski, a nephrologist who is chief health care officer at the Association of American Medical Colleges, or AAMC. “That’s where I see the problem of not having some kind of continuous care.” “We all need care that is coordinated and longitudinal,” said Dr. Michael Munger, president of the American Academy of Family Physicians, who practices in Overland Park, Kan. “Regardless of how healthy you are, you need someone who knows you.” The best time to find that person, Munger and others say, is before a health crisis, not during one. And that may mean waiting weeks. A 2017 survey by physician search firm Merritt Hawkins found that the average wait time for a new-patient appointment with a primary care doctor in 15 large metropolitan areas is 24 days, up from 18.5 days in 2014. While wait times for new patients may reflect a shortage of primary care physicians — in the view of the AAMC — or a maldistribution of doctors, as other experts argue, there is no dispute that primary care alternatives have exploded. There are now more than 2,700 retail clinics in the United States, most in the South and Midwest, according to Rand Corp. researchers. Connecting With Care To attract and retain patients, especially young adults, primary care practices are embracing new ways of doing business. Many are hiring additional physicians and nurse practitioners to see patients more quickly. They have rolled out patient portals and other digital tools that enable people to communicate with their doctors and make appointments via their smartphones. Some are exploring the use of video visits. Mott Blair, a family physician in Wallace, N.C., a rural community 35 miles north of Wilmington, said he and his partners have made changes to accommodate millennials, who make up a third of their practice. “We do far more messaging and interaction through electronic interface,” he said. “I think millennials expect
High-Deductible Health Plans Fall From Grace In Employer-Based Coverage

Jay Hancock, Kaiser Health News With workers harder to find and Obamacare’s tax on generous coverage postponed, employers are hitting pause on a feature of job-based medical insurance much hated by employees: the high-deductible health plan. Companies have slowed enrollment in such coverage and, in some cases, reinstated more traditional plans as a strong job market gives workers bargaining power over pay and benefits, according to research from three organizations. This year, 39 percent of large, corporate employers surveyed by the National Business Group on Health (NBGH) offer high-deductible plans, also called “consumer-directed” coverage, as workers’ only choice. For next year, that figure is set to drop to 30 percent. “That was a surprise, that we saw that big of a retraction,” said Brian Marcotte, the group’s CEO. “We had a lot of companies add choice back in.” Few if any employers will return to the much more generous coverage of a decade or more ago, benefits experts said. But they’re reassessing how much pain workers can take and whether high-deductible plans control costs as advertised. “It got to the point where employers were worried about the affordability of health care for their employees, especially their lower-paid people,” said Beth Umland, director of research for health and benefits at Mercer, a benefits consultancy that also conducted a survey. The portion of workers in high-deductible, job-based plans peaked at 29 percent two years ago and was unchanged this year, according to new data from the Kaiser Family Foundation. (Kaiser Health News is an editorially independent program of the foundation.) Deductibles — what consumers pay for health care before insurance kicks in — have increased far faster than wages, even as paycheck deductions for premiums have also soared. One in 4 covered employees now have a single-person deductible of $2,000 or more, KFF found. Employers and consultants once claimed patients would become smarter medical consumers if they bore greater expense at the point of care. Those arguments aren’t heard much anymore. Because lots of medical treatment is unplanned, hospitals and doctors proved to be much less “shoppable” than experts predicted. Workers found price-comparison tools hard to use. High-deductible plans “didn’t really do what employers hoped they would do, which is create more sophisticated consumers of health care,” Marcotte said. “The health care system is just way too complex.” At the same time, companies have less incentive to pare coverage as Congress has repeatedly postponed the Affordable Care Act’s “Cadillac tax” on higher-value plans. Although deductibles are treading water, total spending on job-based health plans continues to rise much faster than the overall cost of living. That eats into workers’ pay in other ways by boosting what they contribute in premiums. Employer-sponsored group health plans, which insure 150 million Americans — nearly half the country — tend to get less attention than politically charged coverage created by the ACA. For these employer plans, the cost of family coverage went up 5 percent this year and is expected to rise by a similar amount next year, the research shows. Insuring one family in a job-based plan now costs on average $19,616 in total premiums, the KFF data show. The American worker pays $5,547 of that in a country where the median household income is more than $61,000. The KFF survey was published Tuesday; the NBGH data, in August. Mercer has released preliminary results showing similar trends. The recent cost upticks, driven by specialty drug costs and expensive treatment for diseases such as cancer and kidney failure, are an improvement over the early 2000s, when family-coverage costs were rising by an average 7 percent a year. But they’re still nearly double recent rates of inflation and increases in worker pay. Such growth “is unsustainable for the companies I have been working with,” said Brian Ford, a benefits consultant with Lockton Companies, echoing comments made over the decades by experts as health spending has vacuumed up more and more economic resources. For now at least, many large employers can well afford rising health costs. Earnings for corporations in the S&P 500 have increased by double-digit percentages, driven by federal tax cuts and economic growth. Profit margins are near all-time highs. But for workers and many smaller businesses, health costs are a heavier burden. Premiums for family plans have gone up 55 percent in the past decade, twice as fast as worker pay, according to KFF. Employers’ latest cost-control efforts include managing expenses for the most expensive diseases; getting workers to use nurse video-chat services and other types of “telemedicine”; and paying for primary care clinics at work or nearby. At the “top of the list” for many companies are attempts to manage the most expensive medical claims — cases of hemophilia, terrible accidents, prematurely born infants and other diseases — that increasingly cost as much as $1 million each, Umland said. Employers point such patients to the highest-quality doctors and hospitals and furnish guides to steer them through the system. Such steps promise to improve results, reduce complications and save money, she said. On-site clinics cut absenteeism by eliminating the need for employees to drive across town and sit in a waiting room for two hours to get a rash or a sniffle checked or get a vaccine, consultants say. Almost all large employers offer telemedicine, but hardly any workers use it. Thirty-nine percent of the larger companies covering telemedicine now make it comparatively less expensive for workers to consult doctors and nurses virtually, the KFF survey shows. This story originally appeared on Kaiser Health News. Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
