How to Know if You Are Burnt Out: A Travelers’ Guide

By Alex McCoy, Contributing Writer, Owner of Fit Travel Life Burnout is a huge buzzword right now in the nursing community. Honestly, it is nothing new to the field of nursing but it is new that we are learning how to recognize and talk about it more. This is so important because it is bringing this common issue to the forefront of discussions between leadership and making nurses more aware of how to recognize burnout in themselves and others. We need nurses who feel passionate about their jobs and want to show up to work every day, not nurses who are clinging to their position because they simply need an income. Travel nursing is actually one way a lot of staff nurses attempt to combat burnout. The ability to be flexible with your location, change up types of units, and stay out of hospital politics is often a needed reprieve for nurses who are feeling worn down. But does this mean you can’t get burnt out as a travel nurse? Absolutely not. Here are a few questions to ask yourself if you aren’t sure if you are suffering from nursing burnout: Do you dread going to work for every single shift? Sure, there will be days that you would rather be at home binging Netflix or out at the beach instead of working twelve hours in the hospital. But overall you should feel okay with going to work and handling whatever the day will throw at you. If you are at a point where the day before a shift you spend at least 50% or more of your day thinking about how much you don’t want to go to work, you probably need to reevaluate. Is every bump in the road met with a lack of surprise? When you are feeling burnt out, it can be easy to think “of course” every time a doctor is rude to you, you’re running late for work, or you miss out on the contract you were really wanting. It is almost like the extra tension from work spills over into your reaction to everyday things. This can be exhausting mentally to be in such a negative space, so if you are feeling worn out, check how you are handling small upsets. Do you have compassion fatigue? Compassion fatigue is common among healthcare providers because we are exposed to so many tragedies on a daily basis. If you are feeling like it is hard for you to be sympathetic towards your patients, or you are just going through the motions of your basic nursing tasks for the day, it may be a sign that you are suffering from compassion fatigue. Most people become healthcare workers because they want to help and care for others, so feeling this way isn’t normal if you are a caregiver. Are your relationships outside of work affected? All of the exhaustion that comes along with negative inward dialogue and compassion fatigue can bleed over and cause stress in your relationships as well. Whether it is with a friend or a loved one, they may get weary of constant complaints or lack of empathy when they come to you to talk about something important. This can be tricky to identify because someone close to you may not come right out and say you are being negative, or they may assume you are upset with them and be less inclined to talk about the changes they are noticing. However, if you are noticing that it seems like all of your relationships have hit some rocky times, it may be time for you to reflect and see if there is something affecting your interaction with those you care about most. Are you dreading moving or finding a new assignment? When you are working as a travel nurse, part of the excitement is figuring out where you want to go next. Researching fun new neighborhoods, looking up the best local restaurants, and figuring out what to do on your time off is part of the fun. If it comes time to find your next assignment and you are stressing about needing to pack, clean, and move–it may be a sign that you are a little burnt out on the travel nurse lifestyle. Whew. That is a long, heavy topic to cover but once again, it is so important when it comes to longevity in your career and the quality of care you provide your patients. As nurses we give so much to others, and it can be easy to lose track of what we as human beings actually need to make us perform our best. Next week we will dive deeper into how to address burnout once you realize you are feeling overly worn down. Spoiler alert: it does consist of more than bubble baths and pedicures on your days off.
Hospitals Preparing for Flu Season Early: Lock in Your Travel Assignment Now

As the summer months fade and the pandemic continues, healthcare facilities are preparing early for the 2020-2021 flu season and there’s been a steady increase of travel nursing and allied health jobs nationwide. “Hospitals across the country are beginning to bring up concerns of what will happen with the combination of schools opening, COVID and the flu,” said Jennifer Pomietlo, VP of Strategic Development at StaffDNA, the fastest-growing healthcare staffing platform. “They anticipate needing even more travelers due to this and want to be prepared earlier than past years.” Anticipating an influx of patients for both coronavirus and influenza, The New York Times keyed this season as a possible “Twindemic.” Flu season typically peaks between January and February but this year could be very different. During the 2009 swine flu pandemic, the flu peaked by October. If that occurs this year, hospitals could be strained. That is the Director of the Centers for Disease Control and Prevention Dr. Robert Redfield’s biggest fear. Here’s how the possible Twindemic is impacting healthcare travel jobs. Early High Demand Travel nursing and allied health assignments for flu season typically begin posting around October but under the current situation, there is a record number of healthcare jobs, according to StaffDNA’s Job Board, which updates all positions across the country in real-time. Whether located in COVID-19 hotspots or not, hospitals across the country are adding staff to prepare and relieve over-worked staff. The top nursing specialties include ICU, Medical-Surgical, Telemetry and PCU/IMC. Openings for Emergency Room nurses are also ramping up ahead of flu season. Top Travel Nurse Specialties & Highest Pay Packages* RN, ICU 1,050 Unique Jobs Paying up to $4,400/week RN, MS 750 Unique Jobs Paying up to $3,552/week RN, TELE 550 Unique Jobs Paying up to $3,712/week RN, PCU/IMC 325 Unique Jobs Paying up to $3,886/week RN, ER 250 Unique Jobs Paying up to $3,627/week Assignments for Operating Room nurses and surgery-related positions typically increase leading up to the end of the year for elective surgeries. This year, assignments and locations could vary depending on local and state guidelines regarding elective surgeries if there’s another surge in COVID-19 cases and stay-at-home orders. There are also positions open for more focused specialties such as CVICU, Labor & Delivery and Cath Lab RNs. Travelers interested in these roles may need to be more flexible on location to get the higher pay packages. Top Travel Allied Positions* Respiratory Therapist 150 Unique Jobs Paying up to $2,746/week Certified Surgical Technician 175 Unique Jobs Paying up to $2,446/week *Data is according to StaffDNA, the Digital Marketplace for Healthcare Careers, as of 9/8/20. Positions are updated in real-time on the StaffDNA app and Job Board. See all details upfront and personalize pay packages in the app (no registration required).
Flu Season & COVID-19: 5 Tips for Healthcare Travelers Looking for a New Assignment

Summer is over and flu season is quickly approaching. Typically beginning in October through the winter and following spring months, flu season has always been a busy time in healthcare with a high demand for travel nurses and travel allied professionals. This year could look more serious with both COVID-19 and influenza, so hospitals are preparing early for the possible: High influx of patients Potential early peak in flu cases Hospital staff on leave (sick days, PTO, holidays, etc.) Here are 5 things healthcare travelers should keep in mind to help land the best assignment this flu season. #1 Are your Profile & Credentials up-to-date? Healthcare travel jobs that are actively hiring, are also moving quickly. Make sure your professional profile is up-to-date so it can be submitted once a job opens up matching your preferences. Your completed profile includes resume and work experience, licenses, certifications, at least two professional references from within the last 12 months and skills checklist. Hospitals review all profile information to be considered. Whether you’re working with a recruiter or managing the process yourself on a digital platform such as StaffDNA, be proactive. “The market is moving fast; we’ve seen travel positions receive more than 50 submittals within the first couple of hours after a job is posted,” said Jennifer Pomietlo, VP of Strategic Development at StaffDNA, the fastest-growing healthcare staffing platform. “It’s important for healthcare travelers to be diligent and make sure everything is up-to-date so their profile can be one of the first submitted when jobs open up.” #2 How flexible are you on location, pay, etc.? When considering a new travel nursing or allied assignment, it’s crucial to establish your goals and what you’re looking for such as: Location Pay range Hospital setting Travel experience & lifestyle Nearby family or friends As more nurses and allied professionals are looking to travel for the first time and take advantage of higher pay, the more competition there is to fill those highly desirable positions. If your priority is getting the highest pay package, you may need to be more flexible in terms of location and vice versa. If you’re looking to experience a new adventure in a popular travel destination, you may need to be more flexible on the pay rates. #3 What’s Your Specialty? For travel nurses, hospitals typically require at least two years of RN experience in a hospital setting including one year of recent experience in the given specialty. During flu season, specialties such as ICU, MedSurg, Telemetry and ER may be more in demand. Winter months and the end-of-the-year could also bring more scheduled surgeries and a demand for related specialties such as operating room nurses, PACU nurses and certified surgical technicians. Using an app like StaffDNA to set automatic job alerts is helpful to see jobs matching your specialty updated in real-time as hospitals release their needs. #4 Do You Want to Extend? If you’re currently on an assignment you love, travelers can always consider extending their contract—for another 4, 6, 13 weeks or more. This option is usually hassle-free; there’s no onboarding fees or orientation burden. If the hospital is willing and wants to extend your contract, they’re typically more willing to negotiate an increase in pay and time-off requests. #5 Do you have plans for the holidays? Flu season pairs with popular holidays such as Thanksgiving, Christmas and New Year celebrations. If you’re planning on taking any days off, make sure to request your time-off as early as you can. If you’re interviewing for a new assignment, bring it up with the hiring manager at the facility and get the dates added to your contract. If you’re extending, lock in the dates you want off now. It’s important to note that some facilities may require travelers to work at least a certain number of weekends or holidays. Know the policies in place and review your contract details. Without a COVID-19 vaccine released yet, the upcoming flu season remains unknown, but if travelers can lock in their plans for their next assignment now, it’ll be an easier transition before rush. #BONUS TIP: Flu Shots What is your stance on getting a flu shot? The majority of hospitals across the country are being more adamant than ever about travelers getting this season’s flu vaccine before starting their assignment. If you have any restrictions on getting the vaccination, tell your company before applying to jobs so that they can make sure to only submit to openings that do not require it. Read Next: How Declining the Flu Shot Impacts Travel Nurses
AHA Certification Extensions End Oct. 31: Are You Due for a Renewal?

The COVID-19 outbreak brought several modifications for healthcare licensing and certifications. Many emergency responses from several states and hospitals relaxed specific requirements for healthcare professionals so they can continue to work even if they have an expired card or other state license. During stay-at-home orders, many in-person training and testing for healthcare certifications were halted, postponing required renewals for certifications such as BLS, ACLS and PALS. The American Heart Association (AHA) extended renewal deadlines for all provider and instructor certifications for cards that expired in March, April, May and June 2020. These can be renewed for up to 120 days after the recommended “Renew By” date. See below for the specific recommended renewal and extension dates provided by AHA: Recommended “Renew By” Date on Card (end of month) New “Renew By” Due Date with 120- day Extension (end of month) March 2020 July 2020* April 2020 August 2020* May 2020 September 2020 June 2020 October 2020 As of July 23, 2020, AHA announced that it has resumed normal timelines for renewals beginning with cards that expired at the end of July. There is a special exception for affected areas where COVID-19 restrictions are still in place during July and August, at their discretion. Healthcare professionals in these areas may be able to extend the renewal date up to the end of October 2020. These special renewal extensions will end effectively October 31, 2020. By that time, all AHA certifications will need to be up-to-date. The organization said in a statement: “The AHA continues to closely monitor the COVID-19 pandemic and evaluate options for delivering resuscitation education while taking the proper precautions. Our top priority is the safety of both AHA Instructors and learners. We remain committed to serving you as a trusted resource to allow for the continuance of safe, high quality CPR training, as feasible. Thank you for everything you are doing during this challenging time.” There are several flexible options for AHA certification courses being offered that include blended online and hands-on training in small groups. After the virtual training portion, AHA has an easy-to-use tool to find on-site training offered in specific areas. It’s important to note that certification requirements during emergency orders also depend on each healthcare facility’s policies. For example, several hospitals with crisis needs in hot spots are accepting any state RN licenses. Make sure to check the requirements for each assignment you’re submitted to and keep your credentials compliant. Read Next: Travel Healthcare Jobs Hit Record High Since COVID-19 Outbreak
Travel Healthcare Jobs Hit Record High Since COVID-19 Outbreak

This week marks the highest number of nursing jobs reported since the outbreak of COVID-19 earlier this year. Healthcare facilities across the country were forced to furlough or lay off healthcare workers in areas non-related to the virus as a result of the pandemic and the halt of elective surgeries. As states recently reopened, the continued surge in virus cases and restart of routine medical visits and elective surgeries has resulted in a record number of healthcare jobs open in 2020. “The number of nursing and allied health positions on our Job Board has doubled,” said Leah Moss, Account Manager at the leading healthcare staffing platform StaffDNA. “Pre-COVID-19 we were averaging around 4,000 healthcare travel positions. Today, we have more than 7,000 jobs open nationwide. Healthcare facilities that haven’t typically used travel nurses in the past are now calling for help.” ICU nursing specialties remain the highest in demand, especially in hot spots battling the virus such as Florida and Texas. A large portion of the openings are crisis positions with urgent start dates. Other specialties remain high in demand such as Medical-Surgical, Telemetry and PCU/IMC. Here’s the top 10 states with the highest number of nursing jobs. 1. Texas – 714 Unique Jobs RN – ICU: Up to $4,024/wk RN – ER: Up to $3,084/wk RN – MS: Up to $2,966/wk RN – TELE: Up to $2,840/wk RN – PCU/IMC: Up to $2,301/wk RN – OR: Up to $2,139/wk View all Texas Travel Jobs >> 2. Florida – 207 Unique Jobs RN – ICU: Up to $4,028/wk RN – PCU/IMC: Up to $3,816/wk RN – TELE: Up to $2,928/wk RN – ER: Up to $2,166/wk RN – MS: Up to $2,166/wk RN – OR: Up to $1,926/wk View all Florida Travel Jobs >> 3. California – 299 Unique Jobs RN – ICU: Up to $4,400/wk RN – TELE: Up to $4,113/wk RN – PCU/IMC: Up to $3,330/wk RN – MS: Up to $3,263/wk RN – ER: Up to $2,708/wk RN – OR: Up to $2,643/wk View all California Travel Jobs >> 4. Missouri – 237 Unique Jobs RN – PCU/IMC: Up to $3,070/wk RN – OR: Up to $3,012/wk RN – TELE: Up to $2,932/wk RN – ICU: Up to $2,625/wk RN – MS: Up to $2,360/wk RN – ER: Up to $2,229/wk View all Missouri Travel Jobs >> 5. North Carolina – 212 Unique Jobs RN – ICU: Up to $4,02/wk RN – ER: Up to $1,841/wk RN – MS: Up to $3,274/wk RN – TELE: Up to $2,532/wk RN – PCU/IMC: Up to $2,884/wk RN – OR: Up to $2,377/wk View all North Carolina Travel Jobs >> 6. Virginia – 198 Unique Jobs RN – ICU: Up to $3,196/wk RN – OR: Up to $2,139/wk RN – TELE: Up to $2,139/wk RN – ER: Up to $2,118/wk RN – PCU/IMC: Up to $2,211/wk RN – MS: Up to $1,931/wk View all Virginia Travel Jobs >> 7. Tennessee – 198 Unique Jobs RN – ICU: Up to $2,588/wk RN – OR: Up to $2,112/wk RN – TELE: Up to $2,078/wk RN – MS: Up to $2,048/wk RN – ER: Up to $1,841/wk View all Tennessee Travel Jobs >> 8. Arkansas – 130 Unique Jobs RN – ICU: Up to $3,355/wk RN – ER: Up to $2,409/wk RN – PCU/IMC: Up to $2,409/wk RN – MS: Up to $2,337/wk RN – TELE: Up to $2,337/wk RN – OR: Up to $2,221/wk View all Arkansas Travel Jobs >> 9. Georgia – 115 Unique Jobs RN – ER: Up to $3,556/wk RN – ICU: Up to $3,036/wk RN – MS: Up to $2,561/wk RN – PCU/IMC: Up to $2,380/wk RN – OR: Up to $2,370/wk RN – TELE: Up to $2,247/wk View all Georgia Travel Jobs >> 10. South Carolina – 90 Unique Jobs RN – ICU: Up to $3,017/wk RN – PCU/IMC: Up to $2,945/wk RN – TELE: Up to $2,769/wk RN – ER: Up to $2,385/wk RN – MS: Up to $2,351/wk RN – OR: Up to $1,813/wk View all South Carolina Travel Jobs >>
‘Please Tell Me My Life Is Worth A LITTLE Of Your Discomfort,’ Nurse Pleads

Anna Almendrala, KHN.org When an employee told a group of 20-somethings they needed face masks to enter his fast-food restaurant, one woman fired off a stream of expletives. “Isn’t this Orange County?” snapped a man in the group. “We don’t have to wear masks!” The curses came as a shock, but not really a surprise, to Nilu Patel, a certified registered nurse anesthetist at nearby University of California-Irvine Medical Center, who observed the conflict while waiting for takeout. Health care workers suffer these angry encounters daily as they move between treacherous hospital settings and their communities, where mixed messaging from politicians has muddied common-sense public health precautions. “Health care workers are scared, but we show up to work every single day,” Patel said. Wearing masks, she said, “is a very small thing to ask.” Patel administers anesthesia to patients in the operating room, and her husband is also a health care worker. They’ve suffered sleepless nights worrying about how to keep their two young children safe and schooled at home. The small but vocal chorus of people who view face coverings as a violation of their rights makes it all worse, she said. That resistance to the public health advice didn’t grow in a vacuum. Health care workers blame political leadership at all levels, from President Donald Trump on down, for issuing confusing and contradictory messages. “Our leaders have not been pushing that this is something really serious,” said Jewell Harris Jordan, a 47-year-old registered nurse at the Kaiser Permanente Oakland Medical Center in Oakland, California. She’s distraught that some Americans see mandates for face coverings as an infringement upon their rights instead of a show of solidarity with health care workers. (Kaiser Health News, which produces California Healthline, is not affiliated with Kaiser Permanente.) “If you come into the hospital and you’re sick, I’m going to take care of you,” Jordan said. “But damn, you would think you would want to try to protect the people that are trying to keep you safe.” In Orange County, where Patel works, mask orders are particularly controversial. The county’s chief health officer, Dr. Nichole Quick, resigned June 8 after being threatened for requiring residents to wear them in public. Three days later, county officials rescinded the requirement. On June 18, a few days after Patel visited the restaurant, Gov. Gavin Newsom issued a statewide mandate. Meanwhile, cases and hospitalizations continue to rise in Orange County. The county’s flip-flop illustrates the national conflict over masks. When the coronavirus outbreak emerged in February, officials from the U.S. Centers for Disease Control and Prevention discouraged the public from buying masks, which were needed by health care workers. It wasn’t until April that federal officials began advising most everyone to wear cloth face coverings in public. One recent study showed that masks can reduce the risk of coronavirus infection, especially in combination with physical distancing. Another study linked policies in 15 states and Washington, D.C., mandating community use of face coverings with a decline in the daily COVID-19 growth rate and estimated that as many as 450,000 cases had been prevented as of May 22. But the use of masks has become politicized. Trump’s inconsistency and nonchalance about them sowed doubt in the minds of millions who respect him, said Jordan, the Oakland nurse. That has led to a “very disheartening and really disrespectful” rejection of masks. “They truly should have just made masks mandatory throughout the country, period,” said Jordan, 47. Out of fear of infecting her family with the virus, she hasn’t flown to see her mother or two adult children on the East Coast during the pandemic, Jordan said. But a mandate doesn’t necessarily mean authorities have the ability or will to enforce it. In California, where the governor left enforcement up to local governments, some sheriff’s departments have said it would be inappropriate to penalize mask violations. This has prompted some health care workers to make personal appeals to the public. After the Fresno County Sheriff-Coroner’s Office announced it didn’t have the resources to enforce Newsom’s mandate, Amy Arlund, a 45-year-old nurse at the COVID unit at the Kaiser Permanente Fresno Medical Center, took to her Facebook account to plead with friends and family about the need to wear masks. “If I’m wrong, you wore a silly mask and you didn’t like it,” she posted on June 23. “If I’m right and you don’t wear a mask, you better pray that all the nurses aren’t already out sick or dead because people chose not to wear a mask. Please tell me my life is worth a LITTLE of your discomfort?” To protect her family, Arlund lives in a “zone” of her house that no other member may enter. When she must interact with her 9-year-old daughter to help her with school assignments, they each wear masks and sit 3 feet apart. Every negative interaction about masks stings in the light of her family’s sacrifices, said Arlund. She cites a woman who approached her husband at a local hardware store to say he looked “ridiculous” in the N95 mask he was wearing. “It’s like mask-shaming, and we’re shaming in the wrong direction,” Arlund said. “He does it to protect you, you cranky hag!” After seeing a Facebook comment alleging that face masks can cause low oxygen levels, Dr. Megan Hall decided to publish a small experiment. Hall, a pediatrician at the Conway Medical Center in Myrtle Beach, South Carolina, wore different kinds of medical masks for five minutes and then took photos of her oxygen saturation levels, as measured by her pulse oximeter. As she predicted, there was no appreciable difference in oxygen levels. She posted the photo collection on June 22, and it quickly went viral. “Some of our officials and leaders have not taken the best precautions,” said Hall, who hopes for “a change of heart” about masks among local officials and the public. South Carolina Gov. Henry McMaster has urged residents to wear face coverings in public, but he
Hollowed-Out Public Health System Faces More Cuts Amid Virus (KHN)

By Lauren Weber and Laura Ungar and Michelle R. Smith, The Associated Press and Hannah Recht and Anna Maria Barry-Jester The U.S. public health system has been starved for decades and lacks the resources to confront the worst health crisis in a century. Marshaled against a virus that has sickened at least 2.6 million in the U.S., killed more than 126,000 people and cost tens of millions of jobs and $3 trillion in federal rescue money, state and local government health workers on the ground are sometimes paid so little that they qualify for public aid. They track the coronavirus on paper records shared via fax. Working seven-day weeks for months on end, they fear pay freezes, public backlash and even losing their jobs. Since 2010, spending for state public health departments has dropped by 16% per capita and spending for local health departments has fallen by 18%, according to a KHN and Associated Press analysis of government spending on public health. At least 38,000 state and local public health jobs have disappeared since the 2008 recession, leaving a skeletal workforce for what was once viewed as one of the world’s top public health systems. KHN and AP interviewed more than 150 public health workers, policymakers and experts, analyzed spending records from hundreds of state and local health departments, and surveyed statehouses. On every level, the investigation found, the system is underfunded and under threat, unable to protect the nation’s health. Dr. Robert Redfield, the director of the Centers for Disease Control and Prevention, said in an interview in April that his “biggest regret” was “that our nation failed over decades to effectively invest in public health.” So when this outbreak arrived — and when, according to public health experts, the federal government bungled its response — hollowed-out state and local health departments were ill-equipped to step into the breach. Over time, their work had received so little support that they found themselves without direction, disrespected, ignored, even vilified. The desperate struggle against COVID-19 became increasingly politicized and grew more difficult. States, cities and counties in dire straits have begun laying off and furloughing members of already limited staffs, and even more devastation looms, as states reopen and cases surge. Historically, even when money pours in following crises such as Zika and H1N1, it disappears after the emergency subsides. Officials fear the same thing is happening now. “We don’t say to the fire department, ‘Oh, I’m sorry. There were no fires last year, so we’re going to take 30% of your budget away.’ That would be crazy, right?” said Dr. Gianfranco Pezzino, the health officer in Shawnee County, Kansas. “But we do that with public health, day in and day out.” Ohio’s Toledo-Lucas County Health Department spent $17 million, or $40 per person, in 2017. Jennifer Gottschalk, 42, works for the county as an environmental health supervisor. When the coronavirus struck, the county’s department was so short-staffed that her duties included overseeing campground and pool inspections, rodent control and sewage programs, while also supervising outbreak preparedness for a community of more than 425,000 people. When Gottschalk and five colleagues fell ill with COVID-19, she found herself fielding calls about a COVID-19 case from her hospital bed, then working through her home isolation. She stopped only when her coughing was too severe to talk on calls. “You have to do what you have to do to get the job done,” Gottschalk said. Now, after months of working with hardly a day off, she said the job is wearing on her. So many lab reports on coronavirus cases came in, the office fax machine broke. She faces a backlash from the community over coronavirus restrictions and there are countless angry phone calls. Things could get worse; possible county budget cuts loom. But Toledo-Lucas is no outlier. Public health ranks low on the nation’s financial priority list. Nearly two-thirds of Americans live in counties that spend more than twice as much on policing as they spend on non-hospital health care, which includes public health. More than three-quarters of Americans live in states that spend less than $100 per person annually on public health. Spending ranges from $32 in Louisiana to $263 in Delaware, according to data provided to KHN and AP by the State Health Expenditure Dataset project. That money represents less than 1.5% of most states’ total spending, with half of it passed down to local health departments. The share of spending devoted to public health belies its multidimensional role. Agencies are legally bound to provide a broad range of services, from vaccinations and restaurant inspections to protection against infectious disease. Distinct from the medical care system geared toward individuals, the public health system focuses on the health of communities at large. “Public health loves to say: When we do our job, nothing happens. But that’s not really a great badge,” said Scott Becker, chief executive officer of the Association of Public Health Laboratories. “We test 97% of America’s babies for metabolic or other disorders. We do the water testing. You like to swim in the lake and you don’t like poop in there? Think of us.” But the public doesn’t see the disasters they thwart. And it’s easy to neglect the invisible. A History of Deprivation The local health department was a well-known place in the 1950s and 1960s, when Harris Pastides, president emeritus of the University of South Carolina, was growing up in New York City. “My mom took me for my vaccines. We would get our injections there for free. We would get our polio sugar cubes there for free,” said Pastides, an epidemiologist. “In those days, the health departments had a highly visible role in disease prevention.” The United States’ decentralized public health system, which matches federal funding and expertise with local funding, knowledge and delivery, was long the envy of the world, said Saad Omer, director of the Yale Institute for Global Health. “A lot of what we’re seeing right now could be traced back to
Indiana Officially Joins Nurse Licensure Compact (NLC) July 1, 2020
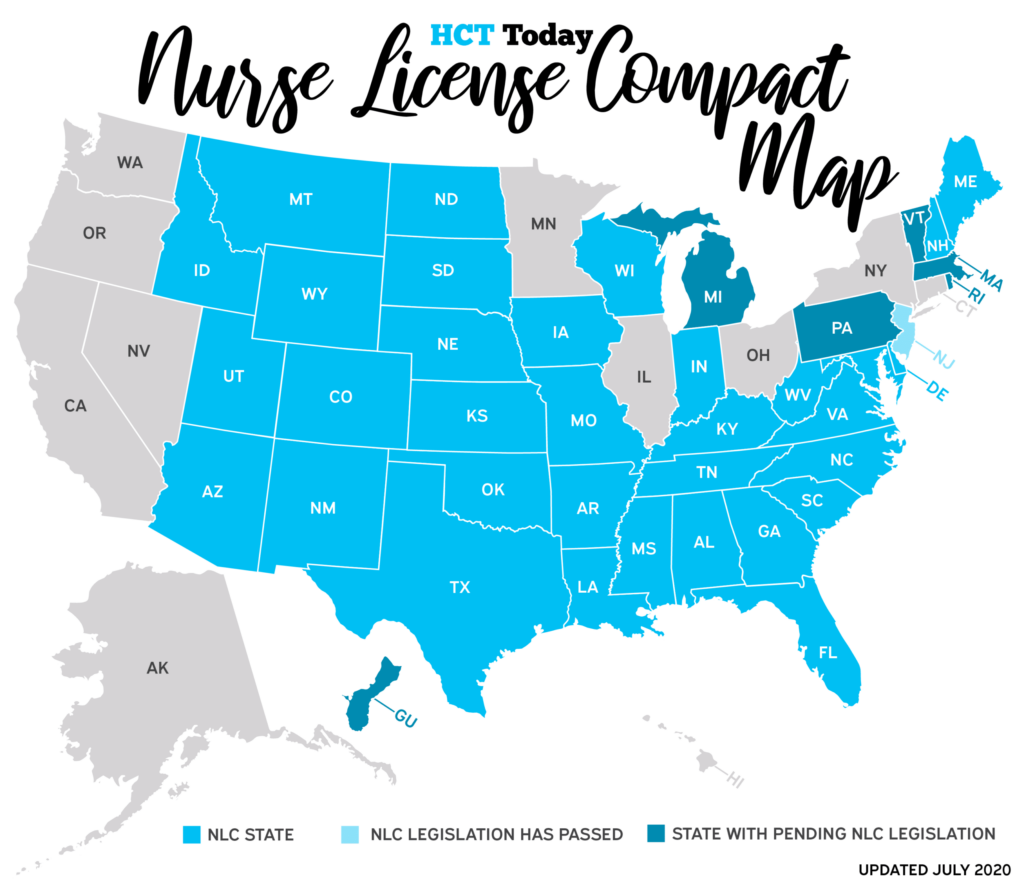
This Wednesday, July 1, 2020, Indiana officially joins 33 other states in implementing the Nurse Licensure Compact (NLC), making it easier for healthcare travelers with compact licenses to work across state lines without having to get separate licenses. Registered nurses and licensed practical/vocational nurses whose primary state of residence is in an NLC state and they hold an active multistate nursing license can now add Indiana to the list of states they can work in. “Indiana has always had several travel nursing needs but the single-state license requirements added a hurdle for travelers who didn’t have an Indiana license to work there,” said Leah Moss, Senior Recruiter at StaffDNA, the fastest-growing digital marketplace for healthcare. “Now, nurses with compact licenses looking for an assignment in Indiana will be able to start quicker and vice versa.” Indiana nursing professionals will be able to apply for a multistate license effective July 1. It’s not necessary for Indiana license holders to wait until their renewal period to apply. The application will be available on the Indiana State Board of Nursing website. In announcement from the NCSBN, Toni Herron from the Indiana State Board of Nursing said: “The NLC presents innovative ways for our Indiana nurses to improve both access to care for patients, while simultaneously reducing the regulatory burden on licensees. This is also great news for nurses who already hold a multistate license from another NLC state, because, as of July 1, 2020, they will be able to practice in Indiana, in person or via telehealth. Our staff looks forward to working with stakeholders to ensure that all Hoosiers, both providers and patients, are fully informed about the dynamic changes on the horizon.” Licensure requirements are aligned in NLC states, so all nurses applying for a multistate license are required to meet the same standards, including submission to federal and state fingerprint-based criminal background checks. For more information, please visit the Indiana State Board of Nursing website. For general information about the NLC, visit the NCSBN NLC webpage.
Tax Season Tips for Healthcare Travelers

By Alex McCoy, Contributing Writer, Owner of Fit Travel Life The season of the year that has accountants working in overdrive and everyone just a little stressed about their finances is upon us: tax season. As a new traveler, this time of year can seem particularly stressful if you are unclear on what you need to do differently as a traveler to make sure all of your finances are in order. Luckily, there isn’t too much difference in the way of actually filing your returns, but it is important to be familiar with tax laws to avoid any issues if you happen to get audited (knock on wood no one reading this has that happen!) Also, I want to note that I am not actually a tax professional–I am simply sharing my experiences and tips to stay a little more organized and get through filing your returns as seamlessly as possible. Tip #1: Have all of your W2’s sent to the same address While some travelers prefer to use mail forwarding services so they can get their hands on their mail without relying on a friend or relative to forward it if you move around during the time when your tax documents are getting mailed out you increase your risk of missing something important. What I have found to be easiest is to make sure all the staffing agencies I work for have the address to my tax home which happens to be my mom’s house. I give her a list of how many W2s I am expecting and what companies they should be coming from. This way she knows when they have all arrived and she can simply send one package with all of my paperwork in it. Tip #2: Keep track of any online payroll logins for the agencies you work for A lot of companies have transitioned to digital versions of tax documents or they do a paper and digital copy. This is actually really handy because you don’t have to wait for your physical mail to make its way to your current location before you can file. The trick comes when it is nine months from the time you signed up for the payroll access and you have no clue what your login might be at the three different agencies you worked for. Head this off by keeping a list somewhere safe of your username and log in for all of your employers, even if you don’t plan on using the site to check your pay stubs regularly. This could save you a lot of time and headache if you can’t track down your W2. Tip #3: Look into using a personal accountant These days it is really easy to get your hands on software that makes filing your taxes by yourself somewhat easy. However, this software might not address specific questions or concerns that come up regarding travel pay or stipends. Because of this I highly recommend looking into a real-live personal accountant. Most of them are familiar with how stipends work (lots of different professions provide living stipends). Plus they can make sure you have all the paperwork to legally collect your stipends and help prevent you from getting into any sticky situations with the IRS. Also, a local accountant is probably a lot cheaper than you would anticipate so don’t let cost be a reason to deter you from hiring someone. Tip #4: Keep a digital or paper trail of any housing payments you make You can read all about how to maintain a tax home here. The key takeaway I want to touch on is that you have to have proof that you are making some sort of housing payment back home and wherever you live on assignment. Even if you are renting a room from your mom back home, you need to make sure to have proof of the payments you are sending. This can be as simple as scheduling a bank transfer or sending a payment via PayPal or Venmo. Most landlords will also use electronic payment methods, but if for some reason you pay cash or use a paper check be sure to get a receipt and keep track of those in case you are audited. Tip #5: Don’t stress With stipends and words like “taxable” or “tax-free” coming into play when you learn about traveler pay, it may seem like filing taxes as a traveler is going to be incredibly complicated. Luckily if you work through an agency as a W2 employee there is not much more to filing than if you work a regular job. There may be more pieces of paper to keep track of since travelers often bounce between agencies, but your agency should take care of deducting proper taxes and all of that ahead of time. Filing taxes as a traveler really isn’t that much different than dealing with tax season as a permanent staff member. Stay organized, hire a professional, and make sure you are maintaining a legal tax home and it should be a smooth process. Alex McCoy currently works as a pediatric travel nurse. She has a passion for health and fitness, which led her to start Fit Travel Life in 2016. She travels with her husband, their cat, Autumn and their dog, Summer. She enjoys hiking, lifting weights, and trying the best local coffee and wine. << Starting a Family as a Traveler
StaffDNA Launches Self-Service Digital Marketplace for the Healthcare Industry
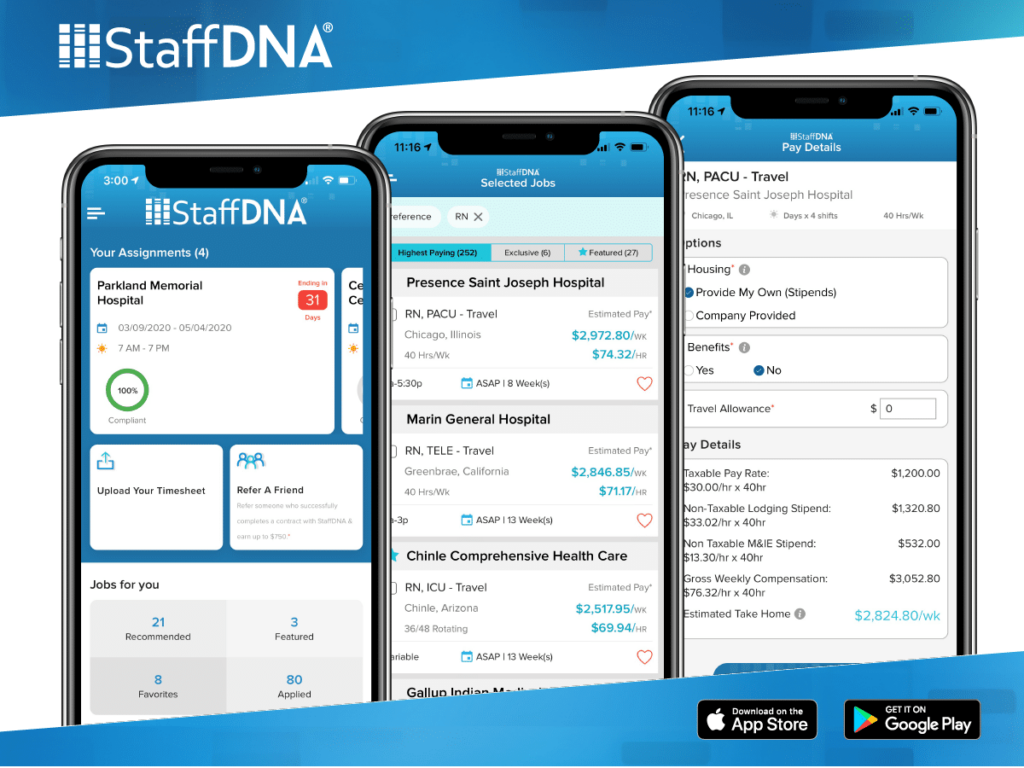
Hospitals, Nurses and Allied Professionals Have a New Digital Platform to Take Control of Finding and Managing Job Placements A first-of-its-kind self-service digital marketplace for healthcare careers was launched this week by StaffDNA, the fast-growing national staffing leader. New StaffDNA technology gives healthcare professionals complete control to find and manage jobs for travel, local and permanent contracts. “The mobile first marketplace is built on top of the most advanced Applicant Tracking System (ATS) in the industry,” said Sheldon Arora, founder and CEO of StaffDNA, “streamlining interactions between professionals and employers in real-time.” “The staffing model has been stagnant for more than 75 years and is inherently inefficient in today’s world,” Arora said. “So, we built one that is going to revolutionize the industry as we know it.” Without having to register, healthcare professionals can search exclusive jobs across the country and get all details upfront—from the charting systems to scrub color requirements. They have the ability to customize pay packages by selecting housing options, benefits, travel allowance, and apply to jobs. With the self-service StaffDNA marketplace, they have the ability to easily manage their assignment details without recruiters: Submit to multiple jobs with 1-click Track job submittal status and get real-time updates Manage compliance requirements, upload credentials and get timely reminders Accept or decline offers, request extensions with the facility Upload timesheets and manage all assignments from past, current and upcoming jobs Founded in 2013, StaffDNA is backed by private investors and leaders in the healthcare, staffing and technology sectors. The company has a strong support team with more than a decade of experience in healthcare staffing including compliance, recruiting, HR, payroll and housing. About StaffDNA Founded by staffing veterans, technology leaders and private investors, StaffDNA has created the new staffing model that gives professionals complete control to find and manage jobs independently—without recruiters or barriers. StaffDNA is the first digital marketplace that completely integrates with ATS software, which allows professionals to connect directly with employers, and get real-time updates. StaffDNA gives healthcare professionals the freedom to find the jobs they want, while making it easier for healthcare facilities to manage their staffing needs more efficiently than ever before. To learn more, visit stage.staffdna.com. StaffDNA’s app is available to download in the Apple App Store and Google Play Store.
