Analysis: Can States Fix The Disaster Of American Healthcare? (KHN)
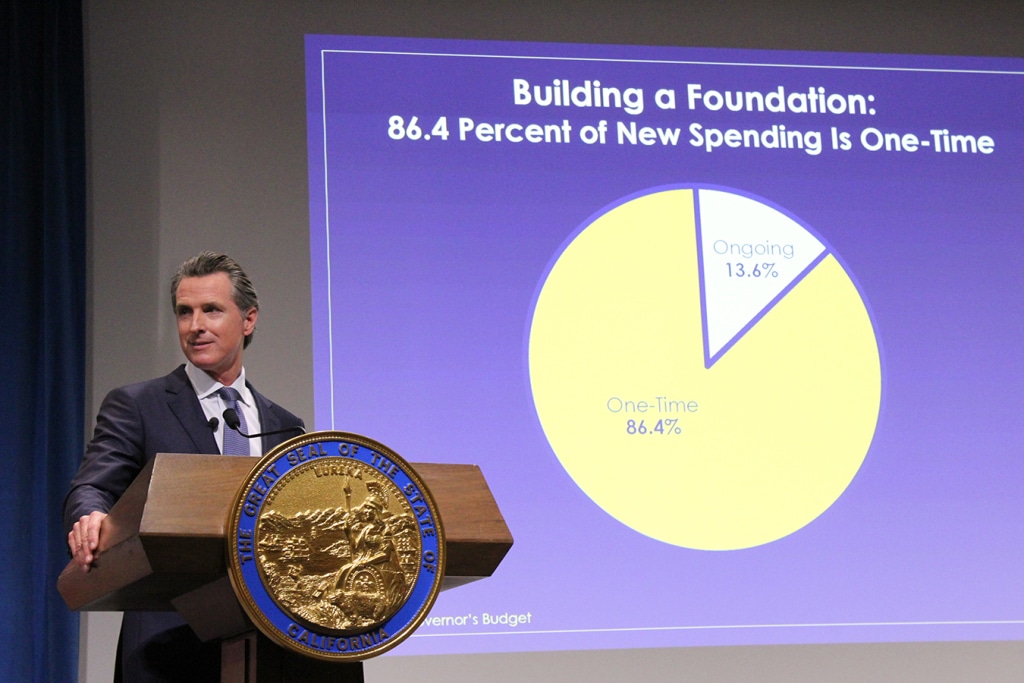
By Elisabeth Rosenthal, Kaiser Health News Last week, California’s new governor, Gavin Newsom, promised to pursue a smörgåsbord of changes to his state’s healthcare system: state negotiation of drug prices, a requirement that every Californian have health insurance, more assistance to help middle-class Californians afford it and healthcare for undocumented immigrants up to age 26. The proposals fell short of the sweeping government-run single-payer plan Newsom had supported during his campaign — a system in which the state government would pay all the bills and effectively control the rates paid for services. (Many California politicians before him had flirted with such an idea, before backing off when it was estimated that it could cost $400 billion a year.) But in firing off this opening salvo, Newsom has challenged the notion that states can’t meaningfully tackle healthcare on their own. And he’s not alone. A day later, Gov. Jay Inslee of Washington proposed that his state offer a public plan, with rates tied to those of Medicare, to compete with private offerings. New Mexico is considering a plan that would allow any resident to buy in to the state’s Medicaid program. And this month, Mayor Bill de Blasio of New York announced a plan to expand healthcare access to uninsured, low-income residents of the city, including undocumented immigrants. For over a decade, we’ve been waiting for Washington to solve our healthcare woes, with endless political wrangling and mixed results. Around 70 percent of Americans have said that healthcare is “in a state of crisis” or has “major problems.” Now, with Washington in total dysfunction, state and local politicians are taking up the baton. The legalization of gay marriage began in a few states and quickly became national policy. Marijuana legalization seems to be headed in the same direction. Could reforming healthcare follow the same trajectory? States have always cared about healthcare costs, but mostly insofar as they related to Medicaid, since that comes from state budgets. “The interesting new frontier is how states can use state power to change the healthcare system,” said Joshua Sharfstein, a vice dean at Johns Hopkins Bloomberg School of Public Health and a former secretary of the Maryland Department of Health and Mental Hygiene. He added that the new proposals “open the conversation about using the power of the state to leverage lower prices in healthcare generally.” Already states have proved to be a good crucible for experimentation. Massachusetts introduced “Romneycare,” a system credited as the model for the Affordable Care Act, in 2006. It now has the lowest uninsured rate in the nation, under 4 percent. Maryland has successfully regulated hospital prices based on an “all payer” system. It remains to be seen how far the West Coast governors can take their proposals. Businesses — pharmaceutical companies, hospitals, doctors’ groups — are likely to fight every step of the way to protect their financial interests. These are powerful constituents, with lobbyists and cash to throw around. The California Hospital Association came out in full support of Newsom’s proposals to expand insurance (after all, this would be good for hospitals’ bottom lines). It offered a slightly less enthusiastic endorsement for the drug negotiation program (which is less certain to help their budgets), calling it a “welcome” development. It’s notable that his proposals didn’t directly take on hospital pricing, even though many of the state’s medical centers are notoriously expensive. Giving the state power to negotiate drug prices for the more than 13 million patients either covered by Medicaid or employed by the state is likely to yield better prices for some. But pharma is an agile adversary and may well respond by charging those with private insurance more. The governor’s plan will eventually allow some employers to join in the negotiating bloc. But how that might happen remains unclear. The proposal by Washington Gov. Inslee to tie payment under the public option plans to Medicare’s rates drew “deep concern” from the Washington State Medical Association, which called those rates “artificially low, arbitrary and subject to the political whims of Washington, D.C.” On the bright side, if Newsom or Inslee succeeds in making healthcare more affordable and accessible for all with a new model, it will probably be replicated one by one in other states. That’s why I’m hopeful. In 2004, the Canadian Broadcasting Corp. conducted an exhaustive nationwide poll to select the greatest Canadian of all time. The top-10 list included Wayne Gretzky, Alexander Graham Bell and Pierre Trudeau. No. 1 is someone most Americans have never heard of: Tommy Douglas. Douglas, a Baptist minister and left-wing politician, was premier of Saskatchewan from 1944 to 1961. Considered the father of Canada’s health system, he arduously built up the components of universal healthcare in that province, even in the face of an infamous 23-day doctors’ strike. In 1962, the province implemented a single-payer program of universal, publicly funded health insurance. Within a decade, all of Canada had adopted it. The United States will presumably, sooner or later, find a model for healthcare that suits its values and its needs. But 2019 may be a time to look to the states for ideas rather than to the nation’s capital. Whichever state official pioneers such a system will certainly be regarded as a great American. This story originally appeared on Kaiser Health News, and also ran in the New York Times. Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
Healthcare Tops Guns, Economy As Voters’ Top Issue

By Phil Galewitz, Kaiser Health News Healthcare has emerged as the top issue for voters headed into the midterm elections, but fewer than half of them say they are hearing a lot from candidates on the issue, according to a new poll released Thursday. Seven in 10 people list healthcare as “very important” as they make their voting choices, eclipsing the economy and jobs (64 percent), gun policy (60 percent), immigration (55 percent), tax cuts (53 percent) and foreign policy (51 percent). When asked to choose just one issue, nearly a third picked health care, according to the survey by the Kaiser Family Foundation. (KHN is an editorially independent program of the foundation.) Still, midterm elections are traditionally a referendum on the president and his party, and that holds true this year as two-thirds of voters say a candidate’s support or opposition to President Donald Trump will be a major factor in their voting decision, the poll found. Health care was also the top issue chosen overall by voters living in areas identified in the survey as political battlegrounds, although the results varied when pollsters drilled down to political parties. Nearly 4 in 10 Democratic battleground voters and 3 in 10 independents chose health care as their most important issue in voting for Congress. Among Republican voters, immigration was their top issue, garnering 25 percent compared with 17 percent for health care. The poll results in two battleground states — Florida and Nevada — also underscored voters’ interest for keeping the Affordable Care Act’s protections for people with preexisting conditions, one of the most popular provisions in the law. Democrats have made that a key part of their campaign, pointing to Republicans’ votes to repeal the entire law and trying to drive home the message that the GOP’s efforts would strip that guarantee. Nonetheless, Republicans have recently sought to fight back on that issue, promising on the stump and in campaign ads that they understand the need to keep the protections and would work to do that. Nearly 7 in 10 Florida voters said they are more likely to vote for a candidate who wants to maintain the protections for people with preexisting conditions, while 9 percent said they are more likely to vote for a candidate who wants to eliminate these protections. In Nevada, nearly 70 percent of voters also said they wanted the ACA preexisting protections guaranteed. In Florida, where the deadliest mass school shooting in American history took place last February, health care also was the top issue among voters. Twenty-six percent of Florida voters listed health as their top issue. The economy and gun policy tied for the second-biggest issue at 19 percent. The shooting at Marjory Stoneman Douglas High School in Parkland, Fla., left 17 students and staff members dead, spurred massive marches around the country and stirred national debate on gun policy. Florida is traditionally a key battleground state but more so this year with close races for the U.S. Senate and governor’s race hanging in the balance. Nearly half of Florida voters said they are more likely to vote for a candidate who wants to expand Medicaid. Florida is one of 17 states that has chosen not to expand Medicaid under the health law, leaving tens of thousands of its adult residents without health insurance. The Republican-controlled legislature has refused to accept millions of dollars in federal funding to extend the coverage. Two in 10 Democratic voters in Florida said support for a candidate supporting a national health plan, or “Medicare-for-all,” is the most important healthcare position for a candidate to take. Andrew Gillum, the Florida Democratic gubernatorial nominee, has said he would support a national health plan. In Nevada, which also has a key Senate battle, the poll found nearly a quarter of voters said health care was the top issue in their decisions this year, but immigration and the economy were very close behind. Nearly a third of Democrats in Nevada said they are looking for a candidate who supports a single-payer health plan. Just under a third of Republicans in Florida and Nevada said that a candidate’s support of repealing the ACA is the most important health issue when they vote. The poll of 1,201 adults was conducted Sept. 19-Oct. 2. The national survey has a margin of error of +/-3 percentage points. This article originally appeared on Kaiser Health News Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
Spurred By Convenience, Millennials Often Spurn The ‘Family Doctor’ Model

By Sandra G. Boodman, Kaiser Health News Calvin Brown doesn’t have a primary care doctor — and the peripatetic 23-year-old doesn’t want one. Since his graduation last year from the University of San Diego, Brown has held a series of jobs that have taken him to several California cities. “As a young person in a nomadic state,” Brown said, he prefers finding a walk-in clinic on the rare occasions when he’s sick. “The whole ‘going to the doctor’ phenomenon is something that’s fading away from our generation,” said Brown, who now lives in Daly City outside San Francisco. “It means getting in a car [and] going to a waiting room.” In his view, urgent care, which costs him about $40 per visit, is more convenient — “like speed dating. Services are rendered in a quick manner.” Brown’s views appear to be shared by many millennials, the 83 million Americans born between 1981 and 1996 who constitute the nation’s biggest generation. Their preferences — for convenience, fast service, connectivity and price transparency — are upending the time-honored model of office-based primary care. Many young adults are turning to a fast-growing constellation of alternatives: retail clinics carved out of drugstores or big-box retail outlets, free-standing urgent care centers that tout evening and weekend hours, and online telemedicine sites that offer virtual visits without having to leave home. Unlike doctors’ offices, where charges are often opaque and disclosed only after services are rendered, many clinics and telemedicine sites post their prices. A national poll of 1,200 randomly selected adults conducted in July by the Kaiser Family Foundation for this story found that 26 percent said they did not have a primary care provider. There was a pronounced difference among age groups: 45 percent of 18- to 29-year-olds had no primary care provider, compared with 28 percent of those 30 to 49, 18 percent of those 50 to 64 and 12 percent age 65 and older. (Kaiser Health News is an editorially independent program of the foundation.) A 2017 survey by the Employee Benefit Research Institute, a Washington think tank, and Greenwald and Associates yielded similar results: 33 percent of millennials did not have a regular doctor, compared with 15 percent of those age 50 to 64. “There is a generational shift,” said Dr. Ateev Mehrotra, an internist and associate professor in the Department of Health Care Policy at Harvard Medical School. “These trends are more evident among millennials, but not unique to them. I think people’s expectations have changed. Convenience [is prized] in almost every aspect of our lives,” from shopping to online banking. So is speed. Younger patients, Mehrotra noted, are unwilling to wait a few days to see a doctor for an acute problem, a situation that used to be routine. “Now,” Mehrotra said, “people say, ‘That’s crazy, why would I wait that long?’” Until recently, the after-hours alternative to a doctor’s office for treatment of a strep throat or other acute problem was a hospital emergency room, which usually meant a long wait and a big bill. Luring Millennials For decades, primary care physicians have been the doctors with whom patients had the closest relationship, a bond that can last years. An internist, family physician, geriatrician or general practitioner traditionally served as a trusted adviser who coordinated care, ordered tests, helped sort out treatment options and made referrals to specialists. But some experts warn that moving away from a one-on-one relationship may be driving up costs and worsening the problem of fragmented or unnecessary care, including the misuse of antibiotics. A recent report in JAMA Internal Medicine found that nearly half of patients who sought treatment at an urgent care clinic for a cold, the flu or a similar respiratory ailment left with an unnecessary and potentially harmful prescription for antibiotics, compared with 17 percent of those seen in a doctor’s office. Antibiotics are useless against viruses and may expose patients to severe side effects with just a single dose. “I’ve seen many people who go to five different places to be treated for a UTI [urinary tract infection] who don’t have a UTI,” said Dr. Janis Orlowski, a nephrologist who is chief health care officer at the Association of American Medical Colleges, or AAMC. “That’s where I see the problem of not having some kind of continuous care.” “We all need care that is coordinated and longitudinal,” said Dr. Michael Munger, president of the American Academy of Family Physicians, who practices in Overland Park, Kan. “Regardless of how healthy you are, you need someone who knows you.” The best time to find that person, Munger and others say, is before a health crisis, not during one. And that may mean waiting weeks. A 2017 survey by physician search firm Merritt Hawkins found that the average wait time for a new-patient appointment with a primary care doctor in 15 large metropolitan areas is 24 days, up from 18.5 days in 2014. While wait times for new patients may reflect a shortage of primary care physicians — in the view of the AAMC — or a maldistribution of doctors, as other experts argue, there is no dispute that primary care alternatives have exploded. There are now more than 2,700 retail clinics in the United States, most in the South and Midwest, according to Rand Corp. researchers. Connecting With Care To attract and retain patients, especially young adults, primary care practices are embracing new ways of doing business. Many are hiring additional physicians and nurse practitioners to see patients more quickly. They have rolled out patient portals and other digital tools that enable people to communicate with their doctors and make appointments via their smartphones. Some are exploring the use of video visits. Mott Blair, a family physician in Wallace, N.C., a rural community 35 miles north of Wilmington, said he and his partners have made changes to accommodate millennials, who make up a third of their practice. “We do far more messaging and interaction through electronic interface,” he said. “I think millennials expect
Hurricane Florence: Online Resources And How To Help

Hurricane Florence was one of the worst storms ever to hit the North Carolina and South Carolina coastline, causing an estimated $17 billion in damages and displacing hundreds of thousands of residents. Disaster relief workers are helping residents pick up the pieces, but there are still ways those outside of the area can help. We’ve compiled a list of online resources that travelers and local residents can use to stay informed and safe during this crisis, as well as how they can help aid disaster relief efforts. We will update this list with new information whenever possible. Click here for our other Hurricane Florence story, which has regular updates about the storm and how state officials and hospitals are responding. Hurricane Safety Checklist Places to Donate or Volunteer Find/Provide Free Disaster Relief Temporary Housing Free Data Recovery For Damaged Computers Free Telehealth Services for Disaster Patients Hurricane Safety Checklist Regardless of where you are located or if you’re working at a hospital during the storm, your first priority is to have a disaster plan in place to protect yourself and your family in a time of crisis. The American Red Cross has provided a hurricane safety checklist that has everything you can do to prepare for the storm and respond to the aftermath. We’ve provided a PDF of the checklist below, but you can also download or view it here: Hurricane Checklist Where You Can Donate and Volunteer American Red Cross The American Red Cross, which will respond to a majority of the crisis areas affected by Hurricane Florence, is currently accepting donations. Donate to American Red Cross here >> Americares Americares is based out of the U.S. but also responds to international crisis areas. They are gathering resources and supplies to support Hurricane Florence relief efforts. Donate to Americares here >> National Voluntary Organizations Active in Disaster (NVOAD) NVOAD is currently accepting donations for Hurricane Florence relief efforts. They have also compiled a list of places where you can connect with volunteer organizations on the ground if you want to directly assist. Find more information or donate here >> Free Temporary Housing (To Use Or Provide) Airbnb Open Homes The Airbnb Open Homes Program is currently providing free temporary housing from Sept. 10 to Oct. 1 for displaced homeowners and relief workers affected by Hurricane Florence. Residents in surrounding areas can also list their homes through the Open Homes program to provide shelter to those in need. If you need to find temporary housing: Create an Airbnb account. Visit this link: https://www.airbnb.com/welcome/evacuees/hurricane-florence-2018 Click the “Find Shelter” button If you want to help provide temporary housing: Create an Airbnb account. Visit this link: https://www.airbnb.com/welcome/evacuees/hurricane-florence-2018 Click the “Sign up your home” button Follow the step-by-step process to place your listing Free Data Recovery TTR Data Recovery, based out of Fairfax, Virginia, is currently offering free data recovery on hard drives and flash media for victims of Hurricane Florence. The company will service any PC owned by users directly affected by the storm and businesses will receive an additional discount, according to their website. Customers may still be responsible for costs of replacement components and shipping, if necessary, and must ship their damaged device no later than Oct. 1. They must also provide proof of residence in South Carolina or North Carolina. For more information on the service, visit their website here: TTR Data Recovery Hurricane Florence Relief Free Telehealth Services These organizations are offering free telehealth services for Hurricane Florence victims, according to Becker’s Hospital Review: Telehealth vendors: American Well MDLive via code “Florence” DoctorOnDemand Teladoc Payers: Anthem via the LiveHealth Online app Capital BlueCross via the Capital BlueCross Virtual Care iOS or Android mobile app Hospitals and health systems: Charleston-based Medical University of South Carolina via code “MUSCFLO,” etv reports. Chapel Hill, N.C.-based UNC Health Care via code “UNCFLORENCE2018” on the UNC Urgent Care 24/7 app Track Hurricane Florence Google has provided a map tool that will let you actively track Hurricane Florence as it moves through the U.S. You can find critical information, like traffic flow or the locations of evacuation resources, by clicking the “Layers” tab and clicking the checkboxes next to things you want to see on the map. Make sure to refresh the page periodically to see the most up-to-date version of the storm’s movement.
Rhode Island Healthcare Workers Strike Begins; Lifespan Spends $10M On Temp Staff

Last-minute negotiations failed for a third time early Monday morning between Providence-based healthcare system Lifespan and healthcare union workers in the midst of a planned 3 p.m. strike. United Nurses and Allied Health Professionals Local 5098 rejected the contract proposal from Providence-based healthcare company Lifespan early Monday morning. The Rhode Island healthcare workers strike is planned to end on July 26 at 3 p.m. Negotiations between Lifespan and the union are scheduled to continue while the strike is underway. “This is a difficult day for all of us,” said UNAP Local 5098 president Frank Sims in a press release. “Lifespan is a broken system where wealthy executives make millions and front line caregivers are ordered to do more with less, and until that changes, patient care will continue to be adversely impacted.” Lifespan officials have planned for the strikes at Rhode Island and Hasbro Children’s hospitals for weeks, hiring temporary workers costing at least $10 million to cover needs at the facilities. The Department of Health activated an “incident command center” to monitor staffing levels, patient care and possible surges due to patient diversions to other hospitals, director Dr. Nicole Alexander-Scott said in a Monday morning press conference. “Rhode Island Hospital’s emergency department will continue to accept all walk-ins,” Alexander-Scott said. “However, EMS throughout the state will only be transporting trauma, burn, cardiac and respiratory arrest and pediatric cases to the Rhode Island Hospital and Hasbro’s hospital EDs. [EMS] will transport other patients to the other hospitals [EDs] throughout the state.” You can view live coverage of the ongoing strikes from the Twitter feed below. This story will be updated as it develops. Tweets by WeAreUNAP
Healthcare Burnout: Why It Happens And How To Avoid It

Healthcare burnout is both regularly talked about among the community and widely studied among academic institutions. Just last week, the Medical Group Management Association (MGMA) released a survey which asked healthcare leaders if they felt burnt out at their job. The results were predictable—45 percent of 1,746 respondents said they feel burnout, 28 percent said they felt “somewhat” burnt out and 27 percent reported no burnout. Healthcare burnout is just as prevalent in the nursing realm, where unsafe staffing ratios, a projected nursing shortage and emotional hurdles create an environment of exhaustion. A quick search of “burnout” on nursing social media forums reveals numerous stories of personal struggles to stay motivated. Addressing this issue is a major concern for industry leaders. Healthcare burnout has a measurable impact on quality of care, costs and safety in healthcare environments, according to a study from the National Academy of Sciences. Travelers have the added challenge of being in a high-burnout profession while also dealing with life on the road, which can sometimes make them feel isolated from their family or peers. But what are the factors that contribute to this, and how can healthcare professionals manage their burnout to avoid quitting? Main factors that contribute to healthcare burnout Studies looking at healthcare burnout have focused on a wide variety of factors, but several large studies have these three in common: High-stress workplace environments Working in healthcare means working in a constantly changing, fast-paced environment. Employees have to adapt to new policies and procedures on a daily basis. Healthcare documenting and treatment technology changes just as quickly. Many healthcare professionals work in literal life-or-death situations where split-second decision making is crucial, so workplace stress is a major issue. Lack of personal agency How many times have you heard someone who works in healthcare say, “I wish I could just take care of my patients instead of dealing with…” or “I feel like my manager doesn’t even listen to what I have to say.” That’s called depersonalization, which refers to the feeling of not being able to focus on providing quality care because of outside forces. Those factors can be a number of different issues like problems with management or even personal conflicts with patients. Many professionals cite issues dealing with confusing or unnecessary documenting programs as a factor of this, although studies show that trend is fading away. Emotional baggage Dealing with sick or dying individuals on a daily basis can impose a heavy emotional toll on healthcare professionals. Violent or aggressive patients can also cause stress, as workplace violence is a major concern in the healthcare industry. According to the Occupational Safety and Health Administration, incidents of serious workplace violence were four times more common in healthcare than in the private industry on average. Ways to avoid healthcare burnout Recognize the signs of burnout early The most dangerous thing you can do as a healthcare professional is ignoring when you feel stressed, overworked, undervalued or exhausted. Knowing the factors of what causes burnout is the first step to addressing those issues. Taking mental breaks to figure out why you are feeling this way can help you identify possible solutions to the problem. You may not be able to take these breaks on the job, so take some time at home to reflect. Consciously avoid distracting activities like watching TV or scrolling through your phone. Plan time for yourself Even the most experienced healthcare worker knows there are some things you can’t control on the job. That’s why it’s important to regularly and intentionally plan your time off to focus on relaxation and recovery. Planning for fun is especially important for travelers as any time off needs to be negotiated through your recruiter before accepting a position at a facility. Experienced travelers also typically take at least one to two months off for vacations, holidays or family time. Talk it out As mentioned by HCT Today contributing writer Natalie Newman, talking about your feelings and experiences with friends, family or professional counselors can help ease the emotional burden of working in healthcare.
As Maine Medicaid expansion stalls, hospitals and enrollees are left in limbo

Maine’s Medicaid-eligible residents, which make up more than 70,000 people, were set to enroll on July 2 as part of the expansion plan approved by nearly 59 percent of voters last November. But after a month of battles between advocacy groups and stonewalling efforts by Gov. Paul LePage’s administration, the enrollment date has passed and hospitals are left waiting for an influx of patients and staffing needs that may not come anytime soon. “A hospital representative I work with said they all have their fingers crossed that [the expansion] gets approved and it all goes smoothly, but she agreed it is a mess currently,” said Larry Jenkins, a sales team member for staffing agency LiquidAgents Healthcare. “There are no plans for additional staff at this time.” For clarity, here’s a timeline of where Maine’s Medicaid expansion plan stands: November 2017: Maine voters approve Medicaid expansion under provisions outlined in the Affordable Care Act, making Maine the first state to approve expansion by referendum. The Maine Department of Health and Human Services is required to file a plan by April 3, 2018 April 3, 2018: No plan is filed by Maine DHHS. LePage said he would not move forward with a plan until adequate funding is approved by the legislature to support expansion efforts. April 30, 2018: Advocacy group Maine Equal Justice Partners sue Maine DHHS to force the administration to submit a plan, citing a $130 million surplus fund that could be used to fund the expansion for 2019. June 4, 2018: Superior Court Justice Michaela Murphy rules in favor of Maine Equal Justice Partners, citing a “complete failure to act” by Maine DHHS in missing the April 3 deadline. They are ordered to submit a plan by June 11. June 7, 2018: LePage’s administration files an appeal for the decision, and requests to not file a plan by June 11 while the appeal is considered. June 18, 2018: Justice Murphy denies the appeal and orders DHHS again to file a plan with the federal government. Gov. LePage’s legal team appeals the order to the Maine Supreme Judicial Court to delay the deadline while the original appeal is considered. Arguments are scheduled for July 18. June 29, 2018: Gov. LePage vetos a potential expansion funding bill. Lawmakers must decide to override or uphold the veto on July 9. July 2, 2018: Maine Equal Justice Partners encourage eligible residents to apply for Medicaid anyways despite ongoing litigation. July 9, 2018: Conservative legislators uphold the veto in an 85-58 House vote. LePage and House Republicans criticize “one-time” funding sources included in the plan, saying Maine needs a long-term funding plan. Monday’s vote on the veto of Maine’s Medicaid expansion funding bill marks the sixth time LePage has stopped expansion legislation through the use of veto during his two terms of office. The final verdict on Maine’s Medicaid expansion efforts may set the precedent for lawmakers in Idaho, Nebraska and Utah. Advocacy groups submitted similar ballot initiatives after successful petitions to let voters decide the fate of Medicaid in their states this November. Utah’s ballot initiative passed state scrutiny and was added to the fall ballot. Secretaries of state in Nebraska and Idaho are reviewing petition signatures to confirm they represent a specific percentage of voters in each state.
National nursing, medical associations decry immigrant family separation

The American Nurses Association and American Medical Association released statements Tuesday asking for President Donald Trump’s administration to end ongoing migrant family separation practices at the U.S. border as quickly as possible. Both organizations said in their statements that forced separations will have “irreparable” negative effects on the physical and mental health of the separated children which could cause long-term health issues. “On behalf of the physician and medical student members of the AMA, I am writing to strongly urge the federal government to withdraw its ‘zero tolerance’ policy that requires the separation of migrating children from their parents or caregivers.” – @CEO_AMA, Dr. James L. Madara. pic.twitter.com/sqf6tZTPpd — AMA (@AmerMedicalAssn) June 20, 2018 “It is well known that childhood trauma and adverse childhood experiences created by inhumane treatment often creates negative health impacts that can last an individual’s entire lifespan,” Dr. James Madara, CEO and executive vice president of the AMA said in a written statement. “Therefore, the AMA believes strongly that, in the absence of immediate physical or emotional threats to the child’s well-being, migrating children should not be separated from their parents or caregivers.” #ICYMI: The ANA urges everyone involved to protect the mental and physical health of these children who face an uncertain future without their families. #FamiliesBelongTogether #WhereAreTheChildren –@anapresident pic.twitter.com/gromaAn4CH — Nurses Association (@ANANursingWorld) June 20, 2018 The ANA urged President Trump’s administration to end forced family separation, reunify the families without delay and establish “compassionate immigration policies.” “The Code of Ethics for Nurses with Interpretive Statements (ANA, 2015) calls on all nurses to always act to preserve the human rights of vulnerable groups such as children, women and refugees,” the ANA statement reads. “The United States of America is better than this. We cannot continue with a policy that is so immoral and cruel to children and families.” Why is this immigrant family separation happening? Attorney General Jeff Sessions announced a zero-tolerance policy towards illegal immigration in April, which required the arrest of any immigrants attempting to illegally enter the U.S. by not using legal border crossing areas. Before, adults who illegally crossed typically faced arrest—except for those who brought along children, as they could not be prosecuted. This undermined the integrity of the immigration system by providing “blanket immunity” for adults who should be legally prosecuted, Sessions said in an opinion piece on USA Today. Since adopting the zero-tolerance policy, at least 2,300 children have been separated from their families as of June 9. Separated children are then sent to Customs and Border Protection facilities, and are later transferred to longer-term care shelters. What’s recently spurned public outcry from human rights organizations and media groups are the three “tender age shelters,” which house many children ages five and under, established in South Texas, the Associated Press learned this week. President Trump signed an executive order Wednesday to put a temporary end to future family separations, but is still pushing for more permanent zero-tolerance legislation.
Medicare Financial Outlook Worsens

Phil Galewitz, Kaiser Health News Medicare’s financial condition has taken a turn for the worse because of predicted higher hospital spending and lower tax revenues that fund the program, the federal government reported Tuesday. In its annual report to Congress, the Medicare board of trustees said the program’s hospital insurance trust fund could run out of money by 2026 — three years earlier than projected last year. A senior government official briefing reporters attributed the worsened outlook for Medicare to several factors that are reducing funding and increasing spending. He said the trustees projected lower wages for several years, which will mean lower payroll taxes, which help fund the program. The recent tax cut passed by Congress would also result in fewer Social Security taxes paid into the hospital trust fund, as some higher-income seniors pay taxes on their Social Security benefits. The aging population is also putting pressure on the program’s finances. In addition, he said moves by the Trump administration and the GOP-controlled Congress to kill two provisions of the Affordable Care Act are also harming Medicare’s future. Those were the repeal of the penalties for people who don’t have insurance and the repeal of an independent board charged with reining in spending if certain financial targets were reached. Marc Goldwein, senior vice president for the nonpartisan Committee for a Responsible Federal Budget, said it was not surprising to see the three-year shift in Medicare’s solvency since the trust fund operates on a narrow margin between revenue and expenses. He said the change to the ACA’s individual mandate penalties, which takes effect next year, is expected to lead to millions more people going without health insurance. That, in turn, will leave hospitals with higher rates of uncompensated care. Some of those expenses are covered by a special Medicare fund paid to hospitals with larger numbers of uninsured patients. The Medicare Part A hospital trust fund is financed mostly through payroll taxes. It helps pay hospital, home health services, nursing home and hospice costs. Medicare Part B premiums — which cover visits to physicians and other outpatient costs — should remain stable next year, the trustees said. About a quarter of Part B costs are paid for by beneficiary premiums with the rest from the federal budget. In a separate report, the government said that Social Security would be able to pay full benefits until 2034, the same estimate as last year. The Social Security Disability Insurance Trust Fund was projected to have sufficient funds until 2032, four years later than forecast last year. Treasury Secretary Steven Mnuchin downplayed any pending crisis, although he acknowledged Medicare faces many long-standing economic and demographic challenges. “Lackluster economic growth in previous years, coupled with an aging population, has contributed to projected shortages for both Social Security and Medicare,” he said in a statement. https://home.treasury.gov/news/press-releases/sm0404 Mnuchin vowed that the Trump administration’s efforts to cut taxes, ease federal regulations and improve trade deals would help both Medicare and Social Security survive over the long term. “Robust economic growth will help to ensure their lasting stability,” he said. Critics, however, doubt the economy will grow fast enough to fix Medicare. The top Democrat on the House Ways & Means Committee, Rep. Richard Neal (Mass.), blamed the Trump administration for Medicare’s deteriorating outlook. “Administration policies in President Trump’s first year have reduced the life of the Medicare trust fund by three years,” he said. “With their repeated efforts to sabotage the nation’s health care system, including their irresponsible tax law, congressional Republicans and President Trump are purposefully running Medicare into the ground.” Seema Verma, administrator of the Centers for Medicare & Medicaid Services, said in a statement the report should spur Congress to act on Trump’s budget plan to cut Medicare spending during the next decade, mostly by reducing payments to doctors, nursing homes and other providers. “These proposals, if enacted, would strengthen the integrity of the Medicare program,” she said. Breaking from tradition, none of the Medicare trustees — which include Mnuchin, Health and Human Services Secretary Alex Azar and Secretary of Labor Alexander Acosta — spoke to the press after releasing the report. A spokesman said they had “scheduling conflicts.” The Medicare trustees said the trust fund will be able to pay full benefits until 2026 but then it will gradually decline to be able to cover 78 percent of expenses in 2039. Medicare provides health coverage to more than 58 million people, including seniors and people with disabilities. It has added 7 million people since 2013. Total Medicare expenditures were $710 billion in 2017. Juliette Cubanksi, associate director of Kaiser Family Foundation’s Medicare Policy Program, cautioned that the report doesn’t mean Medicare is going bankrupt in the next decade but Part A will only be able to pay 91 percent of covered benefits starting in 2026. (KHN is an editorially independent program of the foundation.) She noted that Congress has never let the trust fund go bankrupt. In the early 1970s, the program came within two years of insolvency. But the 2026 estimate marks the closest the program has come to insolvency since 2009, the year before the Affordable Care Act was approved. Joe Baker, president of the Medicare Rights Center, said Congress still has plenty of time to act without making changes that harm beneficiaries. “I worry about fear mongering and the need to do something radical to the program,” he said. Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
The Ebola outbreak is spreading—Here’s how it could affect U.S. travel nurses

UPDATE, 1:51 P.M., MAY 22, 2018: Health officials began a vaccination campaign today to combat the growing Ebola outbreak in the Democratic Republic of Congo, according to a World Health Organization report. With more than 7,500 doses of the vaccine at their disposal, the campaign will first target health workers operating in Ebola virus disease-affected areas, followed by a “ring vaccination” pattern which will focus those who’ve had immediate contact with confirmed Ebola cases. Those who’ve had contact with those contacts will be treated as well, forming a defensive “ring” of vaccinations around each case. More than 600 points of contact have been identified to date, according to the report. The death toll rose to 26 since last week and there are 46 probable, suspected or confirmed cases in the region. Most have been confirmed in Bikoro, but four cases have been confirmed in Mbandaka so far, which prompted a quicker response from health officials because of the city’s size and location. “We need to act fast to stop the spread of Ebola by protecting people at risk of being infected with the Ebola virus, identifying and ending all transmission chains and ensuring that all patients have rapid access to safe, high-quality care,” said Dr Peter Salama, WHO Deputy Director-General for Emergency Preparedness and Response. Original Story DR Congo Health Minister Oly Ilunga Kalenga confirmed a case of Ebola virus disease today in Mbandaka, according to a BBC report. The disease spread to the metropolitan city of about 1 million residents from the rural town of Bikoro about 80 miles away, where the outbreak was officially declared last Wednesday. Since Mbandaka is major transportation hub because of its ease of access to the Congo river and the capital city of Kinshasa, World Health Organization officials say there’s a potential for a rapid increase in new cases. So far, there have been 44 total potential infections in the region, with three confirmed cases of EVD and 41 probable or suspected cases, according to WHO reports. “This is a major development in the outbreak,” senior WHO official Peter Salama told the BBC. “We have urban Ebola, which is a very different animal from rural Ebola. The potential for an explosive increase in cases is now there.” The WHO will discuss the potential of the disease spreading beyond the Congo in an emergency meeting Friday. They will decide whether to declare an international public health emergency, similar to the Western African Ebola outbreak in 2014-16. You can read the full BBC report by clicking here for more details. How it could affect travel nursing jobs in the U.S. If the WHO declares an international health emergency, it could affect policies and procedures at hospitals similar to the recording-breaking 2014-16 outbreak, which saw more than 28,000 confirmed cases of EVD and 11,310 deaths, including two deaths in the U.S. The disease first entered the states on Sept. 30, 2014, after a man who traveled from West Africa to Dallas was confirmed for EVD, according to a CDC report. The man later died from the disease, and two healthcare workers who cared for him later tested positive for the disease, which they recovered from later. During this period, U.S. hospitals adopted new Ebola safety policies at large–especially for Dallas-area facilities–including required Ebola training modules for travel nurses, Travel nursing staff was also required to complete questionnaires about their recent travel history and review forms related to wearing protective equipment. Some hospitals still require prospective travel nurse staff to submit Ebola compliance documents, but it has largely fallen out of practice in the past two years. That could change if hospitals decide to take a more proactive approach in the wake of this outbreak. Staying on top of compliance is already a major hurdle for travel nurses, so adding Ebola compliance requirements will throw another wrench in the works. There’s also the issue of the disease itself, which is highly dangerous because of its ability to spread rapidly through short contact with bodily fluids and its hard-to-detect early stages. You can learn more about EVD diagnoses, preparedness and prevention information on the CDC website.
